Volume 16, Issue 3 (September 2018)
Iranian Rehabilitation Journal 2018, 16(3): 271-288 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Sayadi N, Lotfi Y, Kahlaee A H, Jalilzadeh Afshari P, Bakhshi E. investigation of static Balance control in 4-6 years old children with using the Pediatric Clinical Test of Sensory Interaction for Balance (P-CTSIB). Iranian Rehabilitation Journal 2018; 16 (3) :271-288
URL: http://irj.uswr.ac.ir/article-1-825-en.html
URL: http://irj.uswr.ac.ir/article-1-825-en.html
Nushin Sayadi1 
 , Yones Lotfi *
, Yones Lotfi * 

 1, Amir Hossein Kahlaee2
1, Amir Hossein Kahlaee2 
 , Parisa Jalilzadeh Afshari1
, Parisa Jalilzadeh Afshari1 
 , Enayatollah Bakhshi3
, Enayatollah Bakhshi3 


 , Yones Lotfi *
, Yones Lotfi * 

 1, Amir Hossein Kahlaee2
1, Amir Hossein Kahlaee2 
 , Parisa Jalilzadeh Afshari1
, Parisa Jalilzadeh Afshari1 
 , Enayatollah Bakhshi3
, Enayatollah Bakhshi3 

1- Department of Audiology, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
2- Department of Physiotherapy, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
3- Department of Biostatistics, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
2- Department of Physiotherapy, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
3- Department of Biostatistics, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
Keywords: Postural balance, Children, Balance test, Pediatric Clinical Test of Sensory Interaction for Balance (PCTSIB)
Full-Text [PDF 1120 kb]
(2215 Downloads)
| Abstract (HTML) (4028 Views)
Full-Text: (2426 Views)
1. Introduction
An effective balance control requires combination of vestibular, proprioceptive, and visual system performances [1]. The sensory systems involved in balance control are well-organized and well-developed in adults, thus the balance and postural control are achievable in every situation. However, despite the early anatomical maturation of these systems, they are not functionally developed in children. The functional development of the afferent division of the sensory system, including vestibular, proprioceptive, and visual systems, occurs gradually and hierarchically, and starts after the early maturation of the low-level automatic motor processes [2].
Vestibular disorders are the most common reasons for vertigo in children, with a prevalence rates of 7% to 15%, which may lead to secondary physiological symptoms and avoidant behaviors with negative effects on the child’s academic performance and quality of life [3]. These deficiencies during childhood, can affect the ability to read and study at school [4]. Children with balance problems may face challenges during activities such as playing or getting dressed [5].
Adult standard evaluation methods, which detect the unilateral vestibular disorders, e.g. Videonystagmography (VNG) and caloric testing are challenging and insufferable for children [6, 7]. The rotary chair testing is applied for detecting bilateral vestibular disorders using the natural rotation simulation. This test is very expensive, and is not available in all clinics [8]. Another test to evaluate balance performance is the Sensory Organization Test (SOT) in the Computerized Dynamic Posturography (CDP), which is useful in evaluating patients without postural stability. This test provides a more integrated evaluation of balance performance than the above-mentioned assessments which only examine the vestibulo-ocular reflex. However, it is less used in clinical assessments due to its high cost, long processing time, and large equipment [8].
Considering difficulties in clinical balance assessments, Shumway Cook et al. introduced the Clinical Test of Sensory Interaction on Balance (CTSlB). The CTSlB is the clinical version of the Sensory Organization Test (SOT), useful for the assessment of static balance. This test does not use computerized force plate technology, and is not an expensive instrument. In addition, it has been designed to systematically assess the effects of visual, vestibular, and proprioceptive systems on static balance, and can easily be used in clinical settings [9].
The pediatric version of this test is called the Pediatric Clinical Test of Sensory Interaction for Balance (P-CTSIB). The P-CTSIB reflects the child’s ability to combine and use different information to react in different positions in static balance [10]. Crowe et al. standardized the test process and examined its reliability in 24 children aged 4-9 years without balance disorders. This study indicated a high inter-rater reliability for this test [11].
Other studies showed a high reliability of P-CTSIB in feet-together position among children [12, 13]. Christy et al. also examined the reliability of vestibular functions in children with sensory neural hearing loss compared to healthy children aged 6 to 12 years. They used the Modified Clinical Test of Sensory Interaction in Balance (mCTSIB), which is normally used in adults. In this modified version, the test was performed only in 4 positions (positions 3 and 6 of the P-CTSIB were removed). Their results showed that all of the positions, except position 4 (the hardest position), had a high reliability. Their study also indicated a significant difference in balance performance between this age group and the test [4].
Geldlof et al. performed the test–retest assessment of static and dynamic balance on 20 children aged 9 to 10 years using the limit of stability test and mCTSIB. The results showed a moderate to high reliability for all 4 sensory states of mCTSIB [14]. Although studies indicate the effectiveness of vestibular rehabilitation for children with vestibular hypofunction, the usefulness and effectiveness of vestibular rehabilitations are rarely assessed in these age groups, due to lack of simple and inexpensive clinical tests for children. Given the negative effects of vestibular deficiency on motor performance, postural control, etc. it seems necessary to use simple, valid, and reliable tests with normative data to assess the balance system in children [4]. Therefore, considering the advantages of this test for balance assessment in children and being easy-to-use for clinical settings, also there are no studies using this test in Iran, also considering the limited previous studies in this age group, the current study aimed to evaluate this test in 4-6 years old Iranian children.
2. Methods
A total of 121 children aged 4 to 6 years from some kindergartens in Tehran participated in our study. The participants were selected using the random cluster sampling method. The researcher explained the study objectives and procedure to the parents and they provided the written informed consent. The inclusion criteria consisted of children aged 4 to 6 years, no history of neurological problems, uncorrected visual impairment, developmental motor disorders, and educational problems, based on parental report; Lack of regular exercise, and no use of sedative and efficacious drugs that can affect children’s nervous system and balance system or improve their ability to acquit with the test. The data were collected from different regions, (1 kindergarten in the North, 2 in the West, and 1 in the South of Tehran) during winter 2016.
Initially, the children were explained about the test and the importance of their cooperation. They were reminded about the procedure of the test before each stage, if necessary. The duration of the static balance, the amount of anterior-posterior sway of the body, and lateral sway of the body were evaluated under six different sensory conditions and two different standing positions (feet together and heel-toe position, 12 positions in total).
The combination of three states of visual variables (eyes open, eyes closed, and wearing a visual-conflict dome) and the three states of the support surface variable (standing on a firm surface and a foam) shaped the six sensory situation levels of the test. These six situations were as follows: 1. Standing on a firm surface with eyes open; 2. Standing on a firm surface with eyes closed; 3. Using a visual-conflict dome, standing on a firm surface with eyes open; 4. Standing on a foam with eyes open; 5. Standing on a foam with eyes closed; and 6. Using a visual-conflict dome, and standing on a foam with eyes open (Figure 1).
The children were asked to stand with hands-on-hips and maintain balance for 30 seconds or the occurrence of a new postural adjustment, in all of the test positions. The postural adjustment is a function defined as hands off hips, the movement of one or both feet from the initial position, opening the eyes during the closed-eye condition, or the need of examiner’s assistance to prevent falling [11]. The duration of standing (static balance) and the degrees of lateral sway and anterior-posterior sway were registered. The duration of standing is defined as the start time of the test until the occurrence of a new postural adjustment [11], which was measured in seconds using a chronometer. The maximum standing time was considered 30 seconds to prevent fatigue in children. A sheet in millimeter sizes was placed behind the children to evaluate the amount of sway in a 1×1 m space. The total amount of sway was noted on both sides and on the vertical and horizontal plates.
A laser beam was placed on children’s head using a tensile headband to indicate the frequency of sway on the millimeter plate. The children’s sway rate was determined by beam of the laser mounted on the plate behind them and marked by the examiner. A conflict dome, made by a lantern
An effective balance control requires combination of vestibular, proprioceptive, and visual system performances [1]. The sensory systems involved in balance control are well-organized and well-developed in adults, thus the balance and postural control are achievable in every situation. However, despite the early anatomical maturation of these systems, they are not functionally developed in children. The functional development of the afferent division of the sensory system, including vestibular, proprioceptive, and visual systems, occurs gradually and hierarchically, and starts after the early maturation of the low-level automatic motor processes [2].
Vestibular disorders are the most common reasons for vertigo in children, with a prevalence rates of 7% to 15%, which may lead to secondary physiological symptoms and avoidant behaviors with negative effects on the child’s academic performance and quality of life [3]. These deficiencies during childhood, can affect the ability to read and study at school [4]. Children with balance problems may face challenges during activities such as playing or getting dressed [5].
Adult standard evaluation methods, which detect the unilateral vestibular disorders, e.g. Videonystagmography (VNG) and caloric testing are challenging and insufferable for children [6, 7]. The rotary chair testing is applied for detecting bilateral vestibular disorders using the natural rotation simulation. This test is very expensive, and is not available in all clinics [8]. Another test to evaluate balance performance is the Sensory Organization Test (SOT) in the Computerized Dynamic Posturography (CDP), which is useful in evaluating patients without postural stability. This test provides a more integrated evaluation of balance performance than the above-mentioned assessments which only examine the vestibulo-ocular reflex. However, it is less used in clinical assessments due to its high cost, long processing time, and large equipment [8].
Considering difficulties in clinical balance assessments, Shumway Cook et al. introduced the Clinical Test of Sensory Interaction on Balance (CTSlB). The CTSlB is the clinical version of the Sensory Organization Test (SOT), useful for the assessment of static balance. This test does not use computerized force plate technology, and is not an expensive instrument. In addition, it has been designed to systematically assess the effects of visual, vestibular, and proprioceptive systems on static balance, and can easily be used in clinical settings [9].
The pediatric version of this test is called the Pediatric Clinical Test of Sensory Interaction for Balance (P-CTSIB). The P-CTSIB reflects the child’s ability to combine and use different information to react in different positions in static balance [10]. Crowe et al. standardized the test process and examined its reliability in 24 children aged 4-9 years without balance disorders. This study indicated a high inter-rater reliability for this test [11].
Other studies showed a high reliability of P-CTSIB in feet-together position among children [12, 13]. Christy et al. also examined the reliability of vestibular functions in children with sensory neural hearing loss compared to healthy children aged 6 to 12 years. They used the Modified Clinical Test of Sensory Interaction in Balance (mCTSIB), which is normally used in adults. In this modified version, the test was performed only in 4 positions (positions 3 and 6 of the P-CTSIB were removed). Their results showed that all of the positions, except position 4 (the hardest position), had a high reliability. Their study also indicated a significant difference in balance performance between this age group and the test [4].
Geldlof et al. performed the test–retest assessment of static and dynamic balance on 20 children aged 9 to 10 years using the limit of stability test and mCTSIB. The results showed a moderate to high reliability for all 4 sensory states of mCTSIB [14]. Although studies indicate the effectiveness of vestibular rehabilitation for children with vestibular hypofunction, the usefulness and effectiveness of vestibular rehabilitations are rarely assessed in these age groups, due to lack of simple and inexpensive clinical tests for children. Given the negative effects of vestibular deficiency on motor performance, postural control, etc. it seems necessary to use simple, valid, and reliable tests with normative data to assess the balance system in children [4]. Therefore, considering the advantages of this test for balance assessment in children and being easy-to-use for clinical settings, also there are no studies using this test in Iran, also considering the limited previous studies in this age group, the current study aimed to evaluate this test in 4-6 years old Iranian children.
2. Methods
A total of 121 children aged 4 to 6 years from some kindergartens in Tehran participated in our study. The participants were selected using the random cluster sampling method. The researcher explained the study objectives and procedure to the parents and they provided the written informed consent. The inclusion criteria consisted of children aged 4 to 6 years, no history of neurological problems, uncorrected visual impairment, developmental motor disorders, and educational problems, based on parental report; Lack of regular exercise, and no use of sedative and efficacious drugs that can affect children’s nervous system and balance system or improve their ability to acquit with the test. The data were collected from different regions, (1 kindergarten in the North, 2 in the West, and 1 in the South of Tehran) during winter 2016.
Initially, the children were explained about the test and the importance of their cooperation. They were reminded about the procedure of the test before each stage, if necessary. The duration of the static balance, the amount of anterior-posterior sway of the body, and lateral sway of the body were evaluated under six different sensory conditions and two different standing positions (feet together and heel-toe position, 12 positions in total).
The combination of three states of visual variables (eyes open, eyes closed, and wearing a visual-conflict dome) and the three states of the support surface variable (standing on a firm surface and a foam) shaped the six sensory situation levels of the test. These six situations were as follows: 1. Standing on a firm surface with eyes open; 2. Standing on a firm surface with eyes closed; 3. Using a visual-conflict dome, standing on a firm surface with eyes open; 4. Standing on a foam with eyes open; 5. Standing on a foam with eyes closed; and 6. Using a visual-conflict dome, and standing on a foam with eyes open (Figure 1).
The children were asked to stand with hands-on-hips and maintain balance for 30 seconds or the occurrence of a new postural adjustment, in all of the test positions. The postural adjustment is a function defined as hands off hips, the movement of one or both feet from the initial position, opening the eyes during the closed-eye condition, or the need of examiner’s assistance to prevent falling [11]. The duration of standing (static balance) and the degrees of lateral sway and anterior-posterior sway were registered. The duration of standing is defined as the start time of the test until the occurrence of a new postural adjustment [11], which was measured in seconds using a chronometer. The maximum standing time was considered 30 seconds to prevent fatigue in children. A sheet in millimeter sizes was placed behind the children to evaluate the amount of sway in a 1×1 m space. The total amount of sway was noted on both sides and on the vertical and horizontal plates.
A laser beam was placed on children’s head using a tensile headband to indicate the frequency of sway on the millimeter plate. The children’s sway rate was determined by beam of the laser mounted on the plate behind them and marked by the examiner. A conflict dome, made by a lantern
paper and a total of horizontal and vertical lines inside it, limited the child’s vision from the opposite, up, and down, as well as both sides, in positions 3 and 6 [15] (Figure 2). Two examiners performed the test procedure [11]. The first one marked the sway rate in different directions on the plate behind the children. The second one directed the child and regulated their position correctly, and was also alert to prevent them from falling and recorded the time.
The best response with the longest static balance duration was recorded for the analysis, in all of the 6 conditions for the feet together and heel-toe situation. Between each stage, one minute rest time was given to the children in order to prevent the effect of fatigue.
The test procedure took about 30 minutes. The test was performed in an environment with the least distraction factors so that the child could focus on the balance task. The results were analyzed statistically using SPSS16. Descriptive statistics, repeated measures and post-hoc tests were used for data analysis.
3. Results
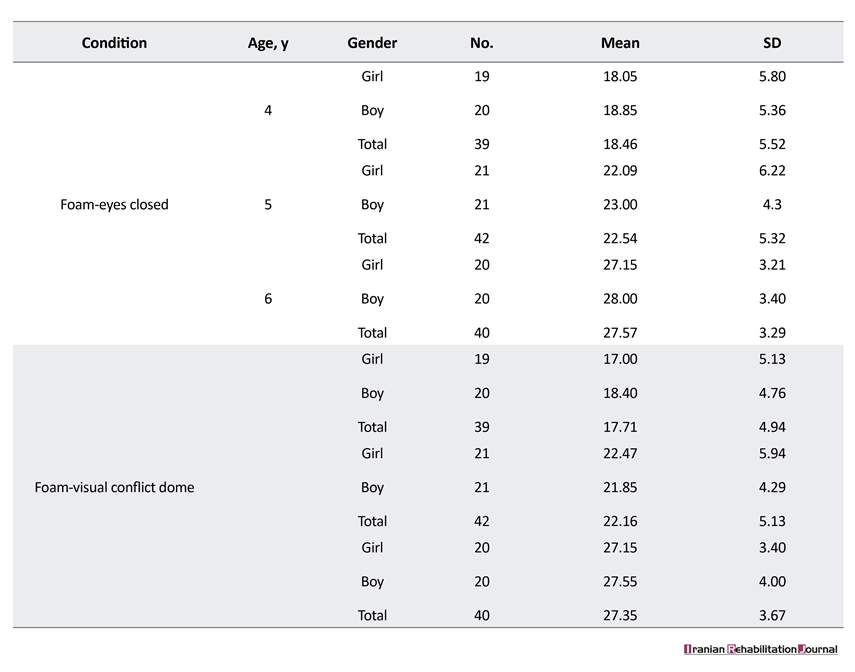
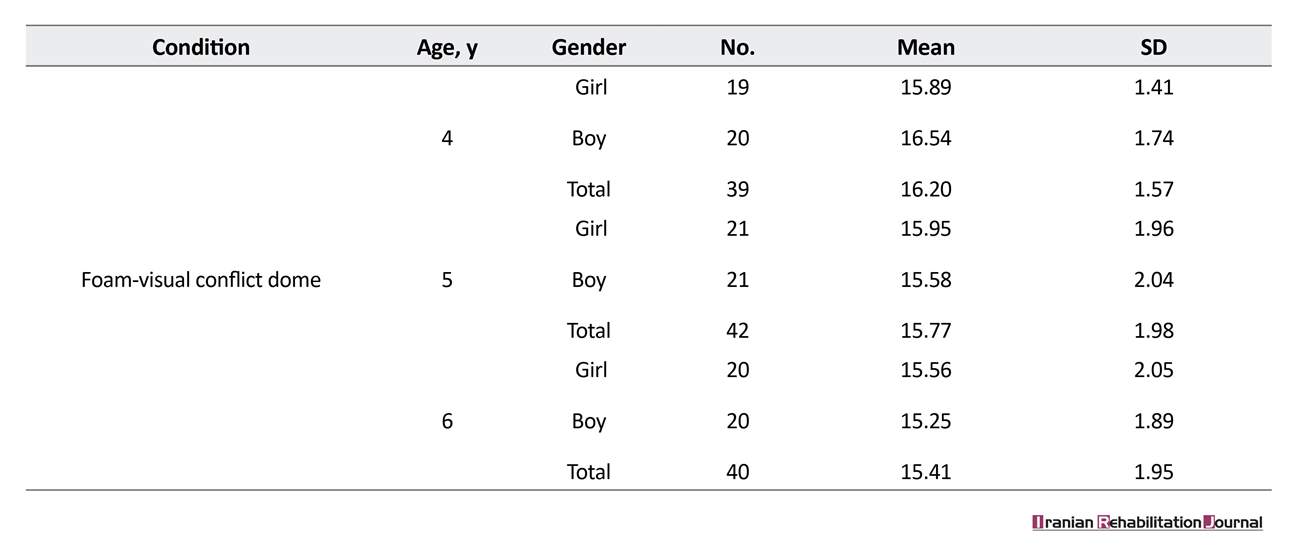
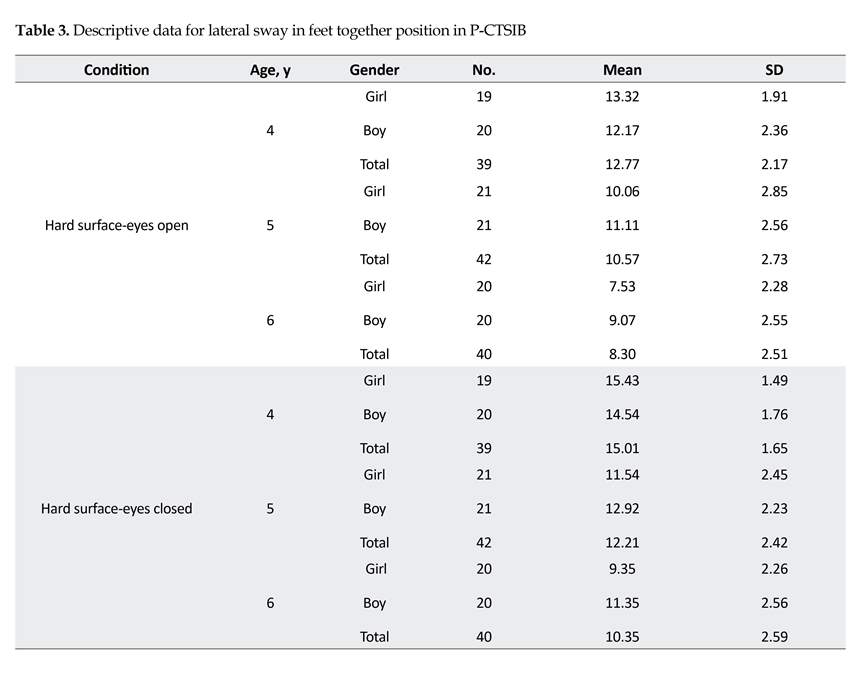
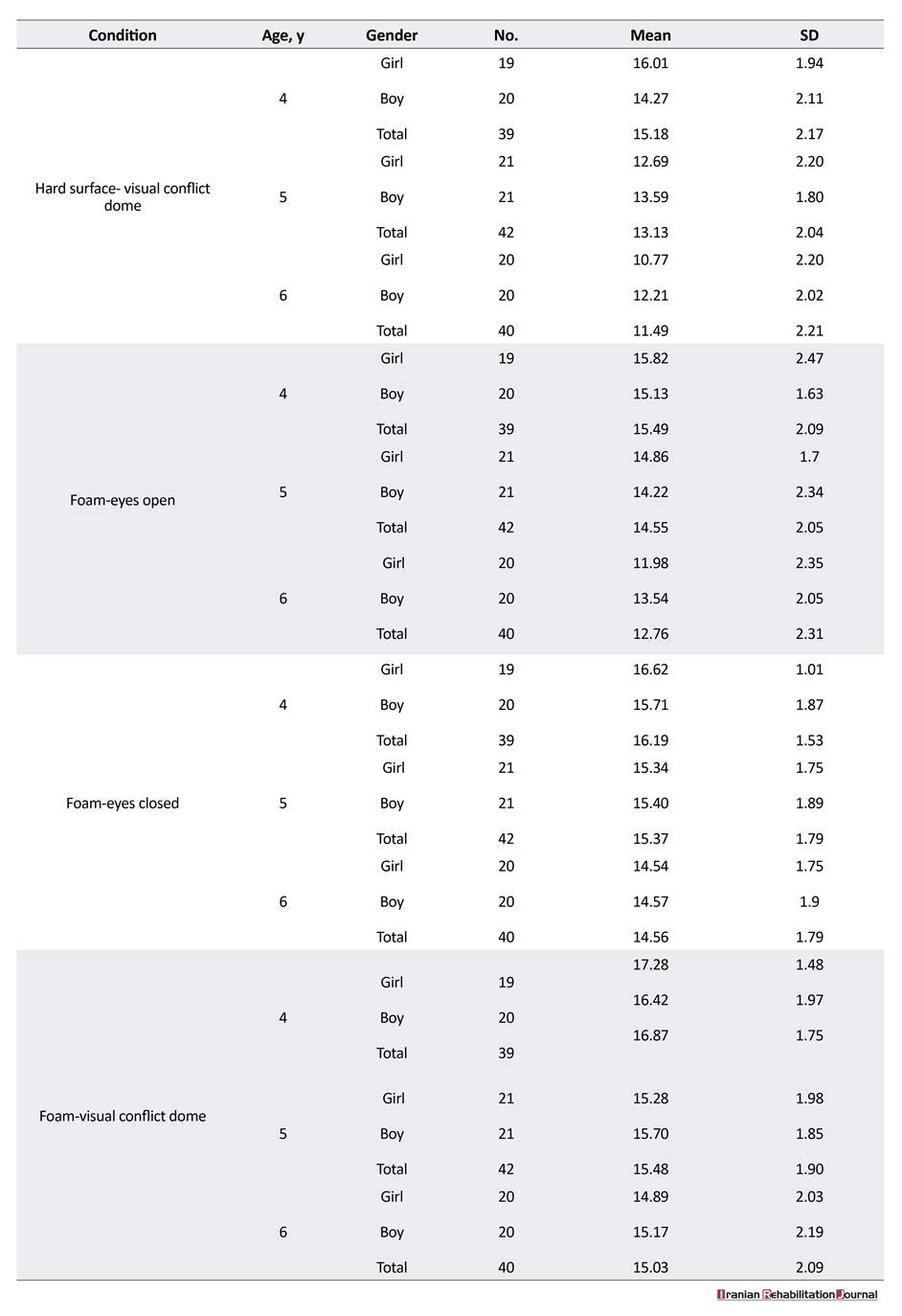
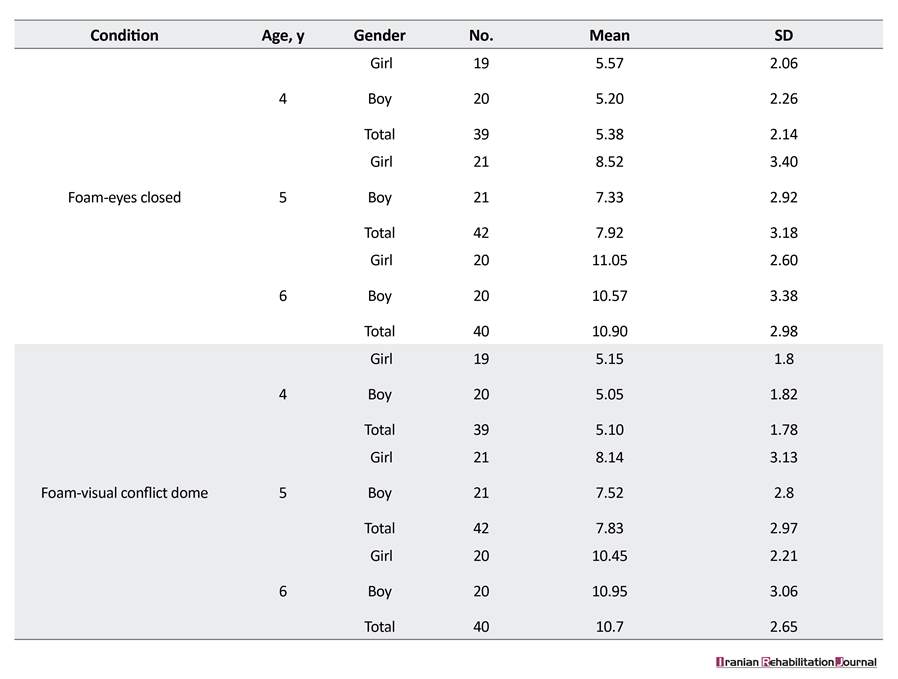
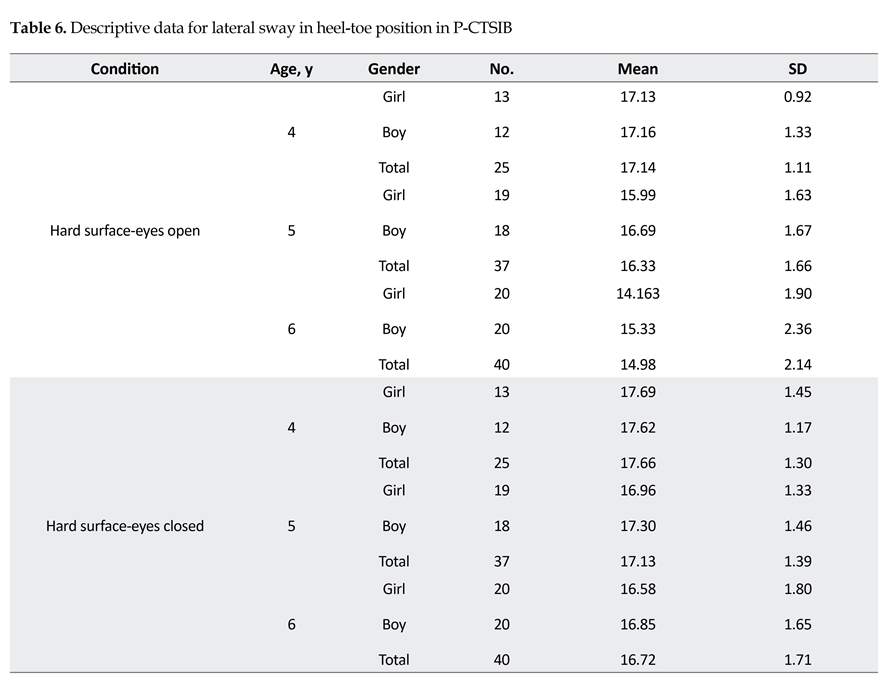
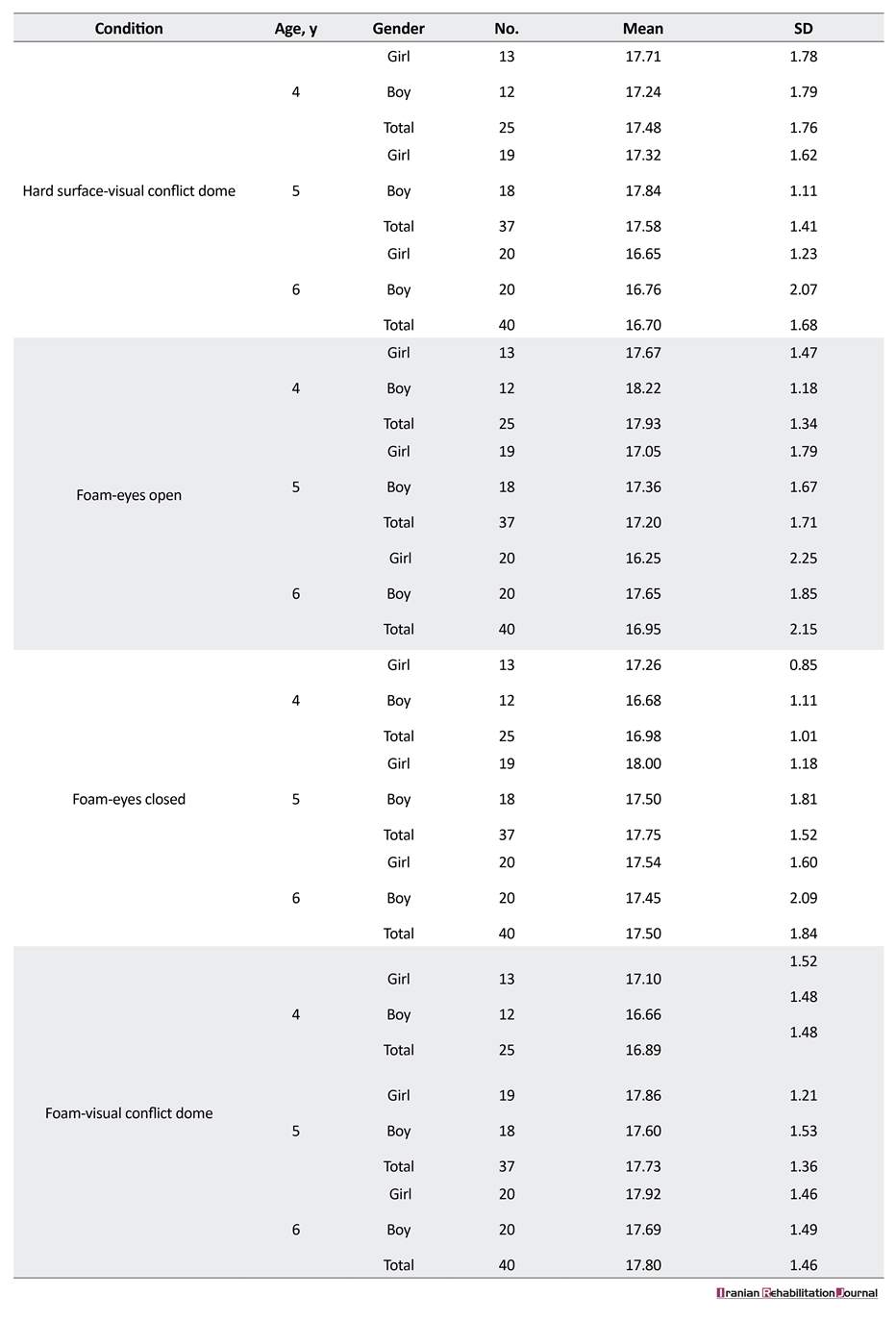
A total of 121 children aged 4-6 years were examined by P-CTSIB test. Descriptive statistics (mean and standard deviations) and repeated measures and post-hoc tests were used for age and gender comparison, performed for the 3 variables of the test, including standing (static balance) duration, anterior-posterior, and lateral sway. Descriptive statistics for standing duration, antero-posterior sway, and lateral sway for feet together position are shown in Tables 1, 2, and 3. As shown, the mean score of standing duration in feet together position increased and the mean score of lateral and AP sway decreased by age.
The best response with the longest static balance duration was recorded for the analysis, in all of the 6 conditions for the feet together and heel-toe situation. Between each stage, one minute rest time was given to the children in order to prevent the effect of fatigue.
The test procedure took about 30 minutes. The test was performed in an environment with the least distraction factors so that the child could focus on the balance task. The results were analyzed statistically using SPSS16. Descriptive statistics, repeated measures and post-hoc tests were used for data analysis.
3. Results
A total of 121 children aged 4-6 years were examined by P-CTSIB test. Descriptive statistics (mean and standard deviations) and repeated measures and post-hoc tests were used for age and gender comparison, performed for the 3 variables of the test, including standing (static balance) duration, anterior-posterior, and lateral sway. Descriptive statistics for standing duration, antero-posterior sway, and lateral sway for feet together position are shown in Tables 1, 2, and 3. As shown, the mean score of standing duration in feet together position increased and the mean score of lateral and AP sway decreased by age.
As shown in Tables 4, 5, and 6, descriptive statistics for standing duration, antero-posterior sway, and lateral sway for heel-toe position, and the mean score of standing duration in heel-toe position increased and the mean score of lateral and AP sway decreased by age. The sample size are smaller in some positions, compared to those reported in Table 4 (duration) because the degree of sway was not measured in some cases (14 four-year-old and 5 five-year-old children) that could not maintain balance for more than 3 seconds.
For analysis of average standing duration, anterior-posterior sway and lateral sway by age and by gender, repeated measures test was used. Analysis of all three items of the test revealed no significant differences (P>0.05) between boys and girls (Table 7).
For analysis of average standing duration, anterior-posterior sway and lateral sway by age and by gender, repeated measures test was used. Analysis of all three items of the test revealed no significant differences (P>0.05) between boys and girls (Table 7).
As shown in Table 8, Analysis of duration, anterior-posterior sway, and lateral sway by age revealed significant differences (P<0.05) on all of three items of the test between the three age groups.
The post-Hoc test and the Tukey test were used to identify differences between the age groups. The Tukey’s post hoc test was used to determine differences in parameters, between the age groups (Table 9). Comparison of average standing duration, anterior-posterior sway and mediolateral sway between age groups revealed significant differences in the three items of the test.
4. Discussion
In the present study, significant differences were found in average standing time, anterior-posterior sway, and lateral sway in different age groups (P<0.05). The bal
The post-Hoc test and the Tukey test were used to identify differences between the age groups. The Tukey’s post hoc test was used to determine differences in parameters, between the age groups (Table 9). Comparison of average standing duration, anterior-posterior sway and mediolateral sway between age groups revealed significant differences in the three items of the test.
4. Discussion
In the present study, significant differences were found in average standing time, anterior-posterior sway, and lateral sway in different age groups (P<0.05). The bal
ance control of the children improved, average standing time increased, and the amount of sway decreased, with increase in age. More significant age differences were found in standing time. Less differences were found in anterior-posterior sway among 4 and 5 year old children.
The study results are in part consistent with those of Richardson et al. (1992) who performed P-CTSIB on 40 children aged 4 and 5 years, and found no significant difference in various positions. However, a significant difference was found between 4 and 5 years old children in position 6 (heel-toe). Overall, the performance of 5-year-old children was better than 4 years old children, in all positions [16].
In contrast, our study found significant difference between the 4 and 5 year olds in all conditions. Such difference can be due to the smaller sample size of the previous study. In our study, fourteen 4 and 5 years old
The study results are in part consistent with those of Richardson et al. (1992) who performed P-CTSIB on 40 children aged 4 and 5 years, and found no significant difference in various positions. However, a significant difference was found between 4 and 5 years old children in position 6 (heel-toe). Overall, the performance of 5-year-old children was better than 4 years old children, in all positions [16].
In contrast, our study found significant difference between the 4 and 5 year olds in all conditions. Such difference can be due to the smaller sample size of the previous study. In our study, fourteen 4 and 5 years old
children could not control their balance for more than 3 seconds in the 5 and 6 heel-toe positions.
This result is in line with the study by Richardson, conducted on forty 4 and 5 years old children, in which only 6 could keep their balance for more than 3 seconds in the 5 and 6 heel-toe positions. A possible explanation can be that, visual input and proprioception are incorrect or removed, in positions 5 and 6. Therefore, children must control their balance only by relying on the vestibular system that is not properly mature in this age. Also, these positions and especially the heel-toe position are the most difficult parts of the test. According to Richadson, there seems to be a development in the selection of sensory strategies for balance control in difficult balance
This result is in line with the study by Richardson, conducted on forty 4 and 5 years old children, in which only 6 could keep their balance for more than 3 seconds in the 5 and 6 heel-toe positions. A possible explanation can be that, visual input and proprioception are incorrect or removed, in positions 5 and 6. Therefore, children must control their balance only by relying on the vestibular system that is not properly mature in this age. Also, these positions and especially the heel-toe position are the most difficult parts of the test. According to Richadson, there seems to be a development in the selection of sensory strategies for balance control in difficult balance
positions at ages 4 to 6. This development seems to occur for few 4 to 5 years old children [16].
Our results are consistent with those of Deitz et al. (1991) who examined balance performance with P-CTSIB on 109, 6 to 9 years old children in the heel-toe and feet-together positions. It could be concluded that older children can keep their balance better in difficult sensory conditions [5]. Also, there was a significant difference in the frequency of sway and standing time between the 4-year-old and 6-year-old children in our study. Performing the heel-toe position was also harder
Our results are consistent with those of Deitz et al. (1991) who examined balance performance with P-CTSIB on 109, 6 to 9 years old children in the heel-toe and feet-together positions. It could be concluded that older children can keep their balance better in difficult sensory conditions [5]. Also, there was a significant difference in the frequency of sway and standing time between the 4-year-old and 6-year-old children in our study. Performing the heel-toe position was also harder
for children in the Deitz’s study which is in line with our results [5].
A study conducted by Sunderraj et al. (2010) on healthy children aged 7-12 years showed that the subjects used the support base in all directions, as CTSIB score increased. This result is in line with our study that indicated CTSIB score increases and balance control ability improves with age [9]. Therefore, improving in postural control ability is a result of proprioceptive, visual and vestibular system development. Thus, researchers should study this test in different age groups and compare the results, in order to determine the developmental effects.
There was no significant gender difference in average standing time, anterior-posterior sway, and lateral sway. This suggests that the study population follow the same developmental path for balance control, and there are similar interactions between vestibular, proprioceptive, and visual systems in both genders. Richardson et al. also found no significant gender difference in P-CTSIB scores [16]. Limited studies investigated the difference between genders on this test in children.
Some limitations of this study included prolonged testing and child’s tiredness. This study designed measurement tools for measuring postural sway in clinical settings. Applying more accurate tools like ours is recommended for the exact measurement of postural sway with the same advantages of easiness, simplicity, and inexpensiveness.
5. Conclusion
The P-CTSIB with feet-together position can be easily performed by 4 to 6 years old children without balance deficiencies. This is a simple and inexpensive test and can be easily used in clinics to assess balance control in children. Given the study limitations, further studies should focus on the heel-toe position in this age group, and the findings of this test should be examined in children with related balance disorders.
Ethical Considerations
Compliance with ethical guidelines
Ethical issues including informed consent, plagiarism, misconduct, data falsification, double publication or submission have been completely observed by the authors.
Funding
The current study was part of MSc. thesis by Nushin Sayadi (Register No:931681003) at the University of Social Welfare and Rehabilitation Sciences. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors certify that they have no affiliation with or involvement in any organization or entity with any financial, or non-financial interest in the subject matter or materials dismissed in this manuscript.
Acknowledgements
The authors appreciate the experts of the Welfare Organization of Tehran, and the study participants’ parents for their cooperation.
References
A study conducted by Sunderraj et al. (2010) on healthy children aged 7-12 years showed that the subjects used the support base in all directions, as CTSIB score increased. This result is in line with our study that indicated CTSIB score increases and balance control ability improves with age [9]. Therefore, improving in postural control ability is a result of proprioceptive, visual and vestibular system development. Thus, researchers should study this test in different age groups and compare the results, in order to determine the developmental effects.
There was no significant gender difference in average standing time, anterior-posterior sway, and lateral sway. This suggests that the study population follow the same developmental path for balance control, and there are similar interactions between vestibular, proprioceptive, and visual systems in both genders. Richardson et al. also found no significant gender difference in P-CTSIB scores [16]. Limited studies investigated the difference between genders on this test in children.
Some limitations of this study included prolonged testing and child’s tiredness. This study designed measurement tools for measuring postural sway in clinical settings. Applying more accurate tools like ours is recommended for the exact measurement of postural sway with the same advantages of easiness, simplicity, and inexpensiveness.
5. Conclusion
The P-CTSIB with feet-together position can be easily performed by 4 to 6 years old children without balance deficiencies. This is a simple and inexpensive test and can be easily used in clinics to assess balance control in children. Given the study limitations, further studies should focus on the heel-toe position in this age group, and the findings of this test should be examined in children with related balance disorders.
Ethical Considerations
Compliance with ethical guidelines
Ethical issues including informed consent, plagiarism, misconduct, data falsification, double publication or submission have been completely observed by the authors.
Funding
The current study was part of MSc. thesis by Nushin Sayadi (Register No:931681003) at the University of Social Welfare and Rehabilitation Sciences. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors certify that they have no affiliation with or involvement in any organization or entity with any financial, or non-financial interest in the subject matter or materials dismissed in this manuscript.
Acknowledgements
The authors appreciate the experts of the Welfare Organization of Tehran, and the study participants’ parents for their cooperation.
References
- Desmond A. Vestibular function: Evaluation and treatment. Stuttgart, Germany: Thieme; 2004.
- Steindl R, Kunz K, Schrott Fischer A, Scholtz A. Effect of age and sex on maturation of sensory systems and balance control. Developmental Medicine and Child Neurology. 2006; 48(6):477-82. [DOI:10.1111/j.1469-8749.2006.tb01299.x] [PMID]
- Pavlou M, Whitney S, Alkathiry AA, Huett M, Luxon LM, Raglan E, et al. The pediatric vestibular symptom questionnaire: A validation study. The Journal of Pediatrics. 2016; 168:171-7.
- Christy JB, Payne J, Azuero A, Formby C. Reliability and diagnostic accuracy of clinical tests of vestibular function for children. Pediatric Physical Therapy. 2014; 26(2):180-9. [DOI:10.1097/PEP.0000000000000039] [PMID]
- Deitz JC, Richardson P, Atwater SW, Crowe TK, Odiorne M. Performance of normal children on the pediatric clinical test of sensory interaction for balance. The Occupational Therapy Journal of Research. 1991; 11(6):336-56. [DOI:10.1177/153944929101100602]
- Wolff DR, Rose J, Jones V, Bloch DA, Oehlert JW, Gamble JG. Postural balance measurements for children and adolescents. Journal of Orthopaedic Research. 1998; 16(2):271-5. [DOI:10.1002/jor.1100160215] [PMID]
- Goebel JA. Should we screen hearing-impaired children for vestibular dysfunction? Archives of Otolaryngology-Head & Neck Surgery. 2003; 129(4):482-3. [DOI:10.1001/archotol.129.4.482] [PMID]
- Hirabayashi SI, Iwasaki Y. Developmental perspective of sensory organization on postural control. Brain and Development. 1995; 17(2):111-3. [DOI:10.1016/0387-7604(95)00009-Z]
- Pandian TJS, Ukamath S, Jetley N, Prabhu R. Clinical Test of Sensory Interaction in Balance (CTSIB): Concurrent validity study in healthy Indian children. Journal of Pediatric Neurology. 2011; 9(03):311-8.
- Gagnon I, Swaine B, Friedman D, Forget R. Children show decreased dynamic balance after mild traumatic brain injury. Archives of Physical Medicine and Rehabilitation. 2004; 85(3):444-52. [DOI:10.1016/j.apmr.2003.06.014] [PMID]
- Crowe TK, Deitz JC, Richardson PK, Atwater SW. Interrater reliability of the pediatric clinical test of sensory interaction for balance. Physical & Occupational Therapy in Pediatrics. 1991; 10(4):1-27. [DOI:10.1080/J006v10n04_01]
- Lotfi Y, Kahlaee AH, Sayadi N, Afshari PJ, Bakhshi E. Test-retest reliability of the pediatric clinical test of sensory interaction for balance in 4-6 years old children. Auditory and Vestibular Research. 2017; 26(4):202-8.
- Westcott SL, Crowe TK, Deitz JC, Richardson PK. Test-retest reliability of the Pediatric Clinical Test of Sensory Interaction for Balance (P-CTSIB). Physical & Occupational Therapy in Pediatrics. 1994; 14(1):1-22. [DOI:10.1080/J006v14n01_01]
- Geldhof E, Cardon G, De Bourdeaudhuij I, Danneels L, Coorevits P, Vanderstraeten G, et al. Static and dynamic standing balance: Test-retest reliability and reference values in 9 to 10 year old children. European Journal of Pediatrics. 2006; 165(11):779-86. [DOI:10.1007/s00431-006-0173-5] [PMID]
- Shumway Cook A, Horak FB. Assessing the influence of sensory interaction on balance: Suggestion from the field. Physical Therapy. 1986; 66(10):1548-50. [DOI:10.1093/ptj/66.10.1548] [PMID]
- Richardson PK, Atwater SW, Crowe TK, Deitz JC. Performance of preschoolers on the pediatric clinical test of sensory interaction for balance. American Journal of Occupational Therapy. 1992; 46(9):793-800. [DOI:10.5014/ajot.46.9.793] [PMID]
Article type: Original Research Articles |
Subject:
Audiology
Received: 2018/03/25 | Accepted: 2018/07/20 | Published: 2018/09/1
Received: 2018/03/25 | Accepted: 2018/07/20 | Published: 2018/09/1
References
1. Desmond A. Vestibular function: Evaluation and treatment. Stuttgart, Germany: Thieme; 2004.
2. Steindl R, Kunz K, Schrott Fischer A, Scholtz A. Effect of age and sex on maturation of sensory systems and balance control. Developmental Medicine and Child Neurology. 2006; 48(6):477-82. [DOI:10.1111/j.1469-8749.2006.tb01299.x] [PMID] [DOI:10.1111/j.1469-8749.2006.tb01299.x]
3. Pavlou M, Whitney S, Alkathiry AA, Huett M, Luxon LM, Raglan E, et al. The pediatric vestibular symptom questionnaire: A validation study. The Journal of Pediatrics. 2016; 168:171-7. [DOI:10.1016/j.jpeds.2015.09.075] [PMID]
4. Christy JB, Payne J, Azuero A, Formby C. Reliability and diagnostic accuracy of clinical tests of vestibular function for children. Pediatric Physical Therapy. 2014; 26(2):180-9. [DOI:10.1097/PEP.0000000000000039] [PMID] [DOI:10.1097/PEP.0000000000000039]
5. Deitz JC, Richardson P, Atwater SW, Crowe TK, Odiorne M. Performance of normal children on the pediatric clinical test of sensory interaction for balance. The Occupational Therapy Journal of Research. 1991; 11(6):336-56. [DOI:10.1177/153944929101100602] [DOI:10.1177/153944929101100602]
6. Wolff DR, Rose J, Jones V, Bloch DA, Oehlert JW, Gamble JG. Postural balance measurements for children and adolescents. Journal of Orthopaedic Research. 1998; 16(2):271-5. [DOI:10.1002/jor.1100160215] [PMID] [DOI:10.1002/jor.1100160215]
7. Goebel JA. Should we screen hearing-impaired children for vestibular dysfunction? Archives of Otolaryngology-Head & Neck Surgery. 2003; 129(4):482-3. [DOI:10.1001/archotol.129.4.482] [PMID] [DOI:10.1001/archotol.129.4.482]
8. Hirabayashi SI, Iwasaki Y. Developmental perspective of sensory organization on postural control. Brain and Development. 1995; 17(2):111-3. [DOI:10.1016/0387-7604(95)00009-Z] [DOI:10.1016/0387-7604(95)00009-Z]
9. Pandian TJS, Ukamath S, Jetley N, Prabhu R. Clinical Test of Sensory Interaction in Balance (CTSIB): Concurrent validity study in healthy Indian children. Journal of Pediatric Neurology. 2011; 9(03):311-8.
10. Gagnon I, Swaine B, Friedman D, Forget R. Children show decreased dynamic balance after mild traumatic brain injury. Archives of Physical Medicine and Rehabilitation. 2004; 85(3):444-52. [DOI:10.1016/j.apmr.2003.06.014] [PMID] [DOI:10.1016/j.apmr.2003.06.014]
11. Crowe TK, Deitz JC, Richardson PK, Atwater SW. Interrater reliability of the pediatric clinical test of sensory interaction for balance. Physical & Occupational Therapy in Pediatrics. 1991; 10(4):1-27. [DOI:10.1080/J006v10n04_01] [DOI:10.1080/J006v10n04_01]
12. Lotfi Y, Kahlaee AH, Sayadi N, Afshari PJ, Bakhshi E. Test-retest reliability of the pediatric clinical test of sensory interaction for balance in 4-6 years old children. Auditory and Vestibular Research. 2017; 26(4):202-8.
13. Westcott SL, Crowe TK, Deitz JC, Richardson PK. Test-retest reliability of the Pediatric Clinical Test of Sensory Interaction for Balance (P-CTSIB). Physical & Occupational Therapy in Pediatrics. 1994; 14(1):1-22. [DOI:10.1080/J006v14n01_01] [DOI:10.1080/J006v14n01_01]
14. Geldhof E, Cardon G, De Bourdeaudhuij I, Danneels L, Coorevits P, Vanderstraeten G, et al. Static and dynamic standing balance: Test-retest reliability and reference values in 9 to 10 year old children. European Journal of Pediatrics. 2006; 165(11):779-86. [DOI:10.1007/s00431-006-0173-5] [PMID] [DOI:10.1007/s00431-006-0173-5]
15. Shumway Cook A, Horak FB. Assessing the influence of sensory interaction on balance: Suggestion from the field. Physical Therapy. 1986; 66(10):1548-50. [DOI:10.1093/ptj/66.10.1548] [PMID] [DOI:10.1093/ptj/66.10.1548]
16. Richardson PK, Atwater SW, Crowe TK, Deitz JC. Performance of preschoolers on the pediatric clinical test of sensory interaction for balance. American Journal of Occupational Therapy. 1992; 46(9):793-800. [DOI:10.5014/ajot.46.9.793] [PMID] [DOI:10.5014/ajot.46.9.793]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |