Volume 22, Issue 4 (December 2024)
Iranian Rehabilitation Journal 2024, 22(4): 701-708 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Aslam S, Rehman S S U, Ilahi N. Effects of Myofascial Release on the Pain and Quality of Life in Patients with Fibromyalgia. Iranian Rehabilitation Journal 2024; 22 (4) :701-708
URL: http://irj.uswr.ac.ir/article-1-2068-en.html
URL: http://irj.uswr.ac.ir/article-1-2068-en.html
1- Department of Physical Therapy and Rehabilitation Sciences, Faculty of Allied Health Sciences, Superior University, Lahore, Pakistan.
2- Department of Physical Therapy, Faculty of Rehabilitation and Allied Health Sciences, Lahore Campus, Riphah International University, Islamabad, Pakistan.
3- Department of Physical Therapy, Faculty of Medical Sciences, Layyah Campus, Government College University Faisalabad, Layyah, Pakistan.
2- Department of Physical Therapy, Faculty of Rehabilitation and Allied Health Sciences, Lahore Campus, Riphah International University, Islamabad, Pakistan.
3- Department of Physical Therapy, Faculty of Medical Sciences, Layyah Campus, Government College University Faisalabad, Layyah, Pakistan.
Full-Text [PDF 467 kb]
(1193 Downloads)
| Abstract (HTML) (5049 Views)
Full-Text: (648 Views)
Introduction
Fibromyalgia (FM) is a syndrome characterized by prolonged multifocal pain. It is associated with sleep instabilities, fatigue, and cognitive dysfunction. Common co-morbid conditions include anger and anxiety. It is the second most common rheumatologic disorder [1]. Though the precise cause of FM is unknown, aberrations of the nervous system concerning the processing of pain may explain the prolonged pain. Patients with FM express hyper-excitability and hyper-responsiveness of the centralized nervous system (central sensitization). Nociceptive provocations from muscular tissue may contribute to FM syndrome [2]. FM is common, with a prevalence of 2% in the general population [3]. Estimates of prevalence and female preponderance vary widely (0.4% to >11% and >90% to <61%, respectively) [4]. Some patients with FM also experience other symptoms like headache, migraine, abdominal pain, and irritable bowel syndrome [5]. In the general population, the prevalence of FM is ominously lower than in communities with certain ailments [6]. There is a weakened threshold to pain by nociceptive receptors, leading to an augmented reaction to mechanical stimulus, intervened by the magnification of CNS signaling. Widespread pain has been a clinical attribute of FM. It is described by an augmented sensitivity to pressure and light touch [7]. Family history of joint problems and working status are significant risk factors for FM [8]. People diagnosed with FM frequently encounter challenges related to their mental and cognitive wellbeing. Issues like disrupted sleep, memory issues, feelings of anxiety, and depression are commonly observed and can significantly affect their quality of life (QoL) [9]. Systemic lupus erythematosus-related variables accompany FM, including photosensitivity, oral ulcers, and secondary Sjögren’s [10]. FM is associated with a 1.54-fold increased risk for inflammatory bowel disease [11]. The severity of pain and deprived mental health status is associated with clinically diagnosed FM [12].
The pharmacological approach to FM treatment includes selective serotonin reuptake inhibitors, tricyclic anti-depressants, anti-epileptic drugs, serotonin-norepinephrine reuptake inhibitors, and muscle relaxants [13]. Moreover, aerobic exercise, education, improving sleep habits, and cognitive-behavioral therapy can be administered as fundamental treatments for addressing all symptoms. Mind-body exercises are advised as principal approaches for managing pain, fatigue, and sleep issues. Mindfulness is recognized as a primary treatment for depression and a supplementary treatment for other symptoms. Additionally, various interventions, such as music therapy, relaxation techniques, warm baths, and localized heat, are suggested as supplementary treatments, depending on the symptoms [14]. Nonsteroidal anti-inflammatory drugs like ibuprofen and diclofenac have not proved their effectiveness as standalone treatments [15]. Moreover, Physical activity, like exercise or leisure physical training, is essential in managing FM [16].
Millions of individuals throughout the world suffer from FM, with women making up the majority of cases. FM drastically lowers their QoL and strains the patient and the healthcare system. As a result, research into alternate therapy modalities is necessary. Despite common usage and popularity, these therapies have shown vague, incomplete, and conflicting results. The rationale of the current study was to investigate the effects of myofascial release therapy on pain and the QoL in patients diagnosed with FM, which will pave the way for more tailored, effective, and comprehensive treatment strategies in the management of FM.
Materials and Methods
Study design and participants
This quasi-experimental study was conducted at the Physiotherapy Department of Shalamar Hospital, Lahore, Pakistan, from January 2019 to July 2019. Twenty-eight male and female patients clinically diagnosed with FM, aged 25 to 45 years, were recruited to participate in this study. Study participants were carefully chosen through a non-probability convenience sampling technique, while the sample size was calculated based on the McGill pain scale of the previous study [17]. The level of confidence was set at 0.95(95%). The statistical power was set at 0.8. Each patient provided written informed consent. Patients meeting the inclusion criteria for this study were those who, during their initial assessment, had been afflicted with moderate to severe pain and reported experiencing activity limitation due to pain for a minimum of one day within the past month. The patients who had a fever, infection, hypotension, respiratory disorder, alteration in cutaneous integrity, and those who had received non-pharmacological therapies were excluded. After initial screening, those meeting predetermined inclusion criteria were divided into two groups.
Study interventions
All patients benefited from standard care, including patient education and passive stretching. Group A included 14 patients who received myofascial release technique for treatment in addition to passive stretching. Group B included 14 patients who received passive stretching alone. Written informed consent was taken from every participant. The treatment program included 12 sessions over 4 weeks, 3 sessions per week performed by an experienced physiotherapist. Each treatment session took 30 minutes. Passive stretching consisted of holding for 30 seconds during each repetition. The myofascial release technique consisted of local stretching of muscles that contained tender points, like erector spinae muscles, utilizing the cross-handed technique in the prone lying position. The strength of pressure was accustomed to the individual subjective feelings of the patient during the application of the technique [18]. After the final treatment session, post-intervention pain and QoL measurements were recorded.
The data were analyzed using SPSS, software, version 21. Statistical significance was established at P≤0.05. Using descriptive statistics, frequency tables, and bar charts were provided to show the summary of group measurements. The normality of the data was assessed by the Shapiro-Wilk test. Age, pain rating index, and total FM impact questionnaire scores were normally distributed (P>0.05), but values of present pain index (PPI) were not normally distributed (P<0.05). Parametric tests were applied to find the change between the groups for variables showing normal distribution. The independent t-test was used on the pain rating index (PRI) of the McGill pain questionnaire (MPQ) and the revised FM impact questionnaire (FIQR). The non-parametric test, the Mann-Whitney test, was used to determine the change between the groups for variables not normally distributed, such as the PPI of the McGill pain questionnaire.
Outcome measures
Pre- and post-intervention pain assessment was done using the McGill pain questionnaire, and QoL was assessed by employing FIQR. MPQ is a tool administrated by the interviewer. It can be used to evaluate the effectiveness and efficacy of interventions for pain and to assess pain qualitatively associated with distinct nociceptive conditions and neuropathic pain disorders. The pain is scored between 0 and 78, where 0 indicates no pain, while higher scores correspond to more severe pain intensity [19]. MPQ has been validated in different languages and is a valid and reliable tool for assessing musculoskeletal pain [20].
FIQR is a self‐reported questionnaire that assesses various elements of extensive FM. The psychometric evaluation of FIQR has shown its consistency and validity in the Japanese population with FM. The questionnaire comprises 21 items gauging three domains: “Function,” which included 9 items; “overall impact” of FM on functioning and severity of symptoms, consisting of two items; and “symptoms,” containing 10 items. Every item is scored on a numeric scoring scale with a score ranging from 0 to 10. The results of each domain are summed up, including the function, which ranges from 0 to 90. Overall impact ranges from 0 to 20, and symptoms vary from 0 to 100. After summing the results for every domain, the domains will be normalized by dividing by 3, 1, and 2, respectively. The overall FIQR score is calculated by three domain scores ranging from 0-100. A reduced score shows a better QoL [21].
Data analysis
Age, PRI, and total FM impact questionnaire scores were normally distributed (P>0.05), while values of PPI were not (P<0.05).
Results
A total of 28 subjects contributed to the study. They were equally divided into two groups. Selected subjects in one group were treated with myofascial release therapy and passive stretching, while the other group was treated with passive stretching alone.
The Mean±SD ages of groups A and B were 33.576.18 and 37.21±5.91 years, respectively.
The male-to-female ratio in group A was 6:8, while in group B, it was 5:9.
Table 1 shows that the Mean±SD pre-treatment score of the PRI in group A was 46.76±10.47, and in group B was 43.36±12.7.
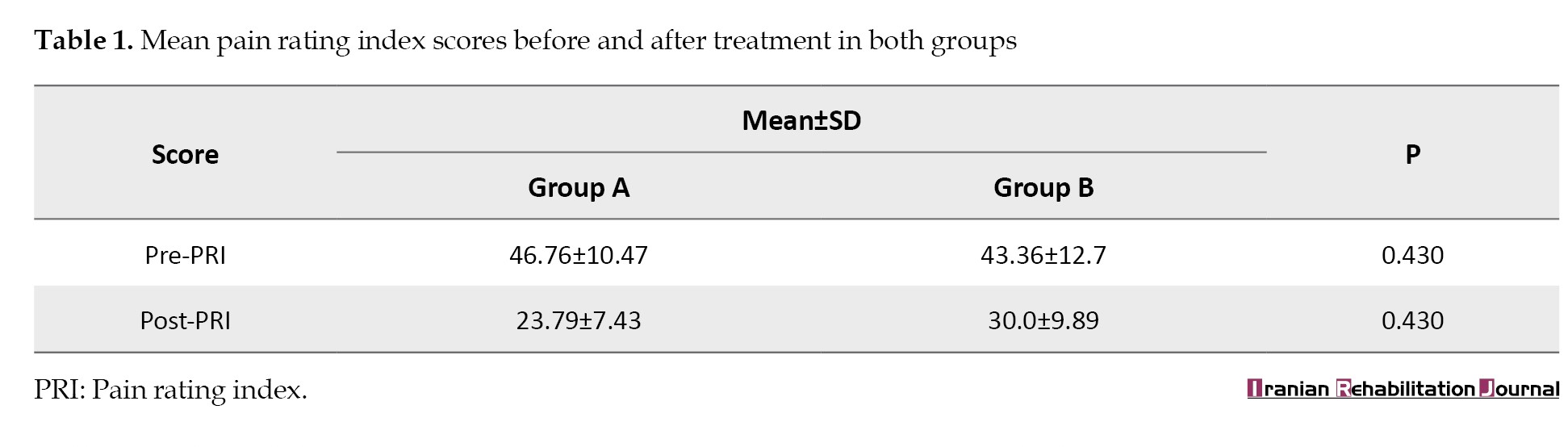
The Mean±SD of the post-treatment score of PRI in group A was 23.79±7.43, and in group B was 30.0±9.89. There was no significant difference in both groups for both pre- and post-PRI scores (P>0.05). Both groups showed equal improvement in PRI scores.
The A and B groups’ Mean±SD pre-treatment PPI scores were observed as 3.21±0.893 and 3.50±1.092 (Table 2).
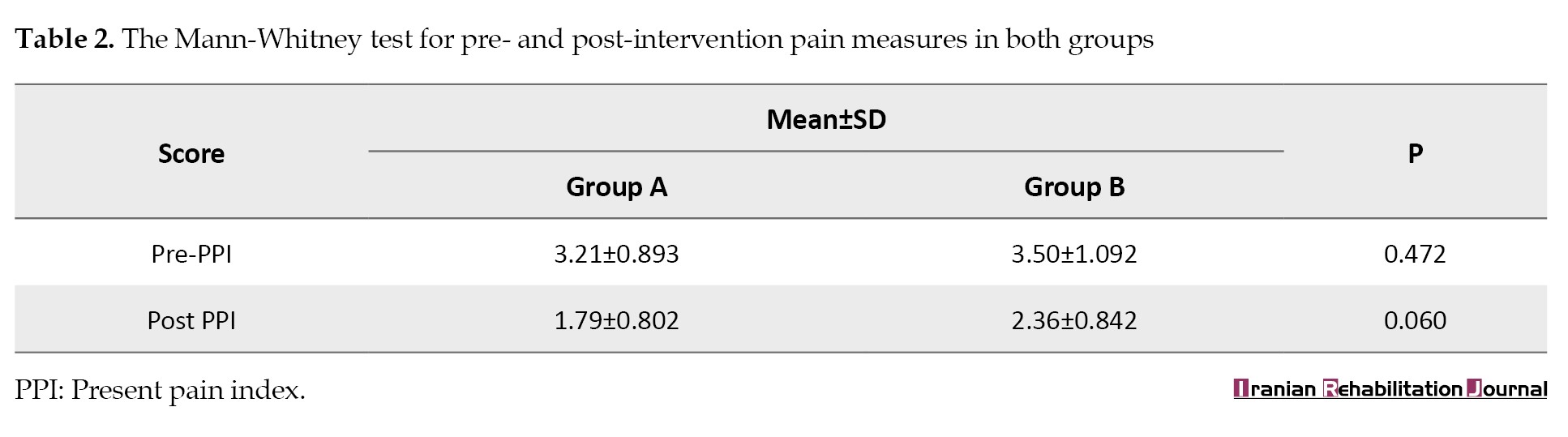
Also, Mean±SD post-treatment PPI scores in group A were 1.79±0.802, and in group B was 2.36±0.842 (P>0.05). In contrast, the difference in the mean scores of the two groups was not statistically significant. Similarly, there was no significant difference in both groups’ pre- and post-treatment scores (P>0.05). Both groups showed equal improvement in PPI scores (Table 2).
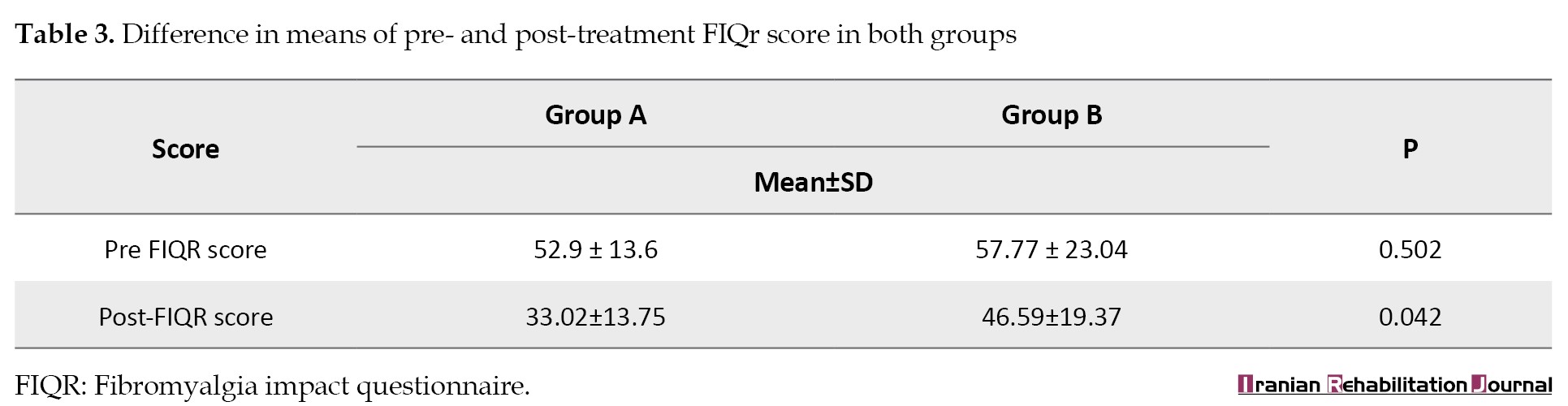
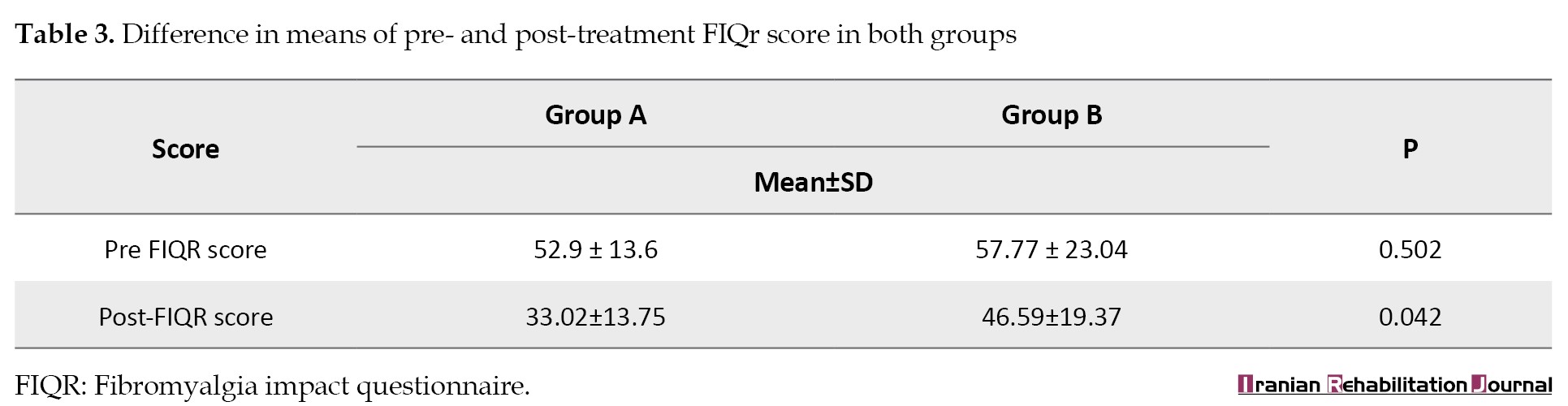
Moreover, the pre-treatment FIQR scores of both groups did not show any significant difference (P>0.05). However, when the mean FIQR scores of post-treatment of the two groups were compared, it revealed a significant difference (P<0.05). More improvement was noted in the FIQR score of group A than in group B (Table 3).
Discussion
The current study determines the effects of the myofascial release technique on pain and QoL in patients with clinically diagnosed FM.
After pre- and post-intervention analysis, there was an improvement in pain in both groups, but there was no significant difference between the groups in terms of pre- and post-scores. The QoL recorded on the FIQR was improved in both groups. However, the difference in the means of post-treatment scores of the two groups was significant, showing that more improvement was noted in the FIQR score of group A, who received myofascial release technique in addition to passive stretching, than in group B, who just received passive stretching.
Similarities with the current study’s findings were reported in an investigation that was intended to discover the advantages of applying self-myofascial release intervention on wellbeing-related to QoL in FM patients, and it concluded that the use of a self-myofascial release program improved the wellbeing life quality of individuals having FM [22].
Our study aligns with a single-blind, randomized controlled trial to compare the impacts of dry needling and myofascial release on FM patients. The study recommended that dry needling is more compelling than myofascial release in addressing pain in FM patients. They highlighted the potential of dry needling as a useful alternative for managing FM symptoms [2].
Similar to the current research findings, a systematic review by Laimi et al. about the efficacy of myofascial release therapy in treating persistent musculoskeletal pain revealed that myofascial release therapy is insufficient for chronic pain [23].
Moreover, varied results were demonstrated by a systematic review conducted by Yuan et al., aimed to evaluate the efficacy of different forms of soft tissue manipulation in treating FM. Compared to a placebo, the myofascial release showed significantly better pain results than the current study. However, similar trends were observed between that systematic review and the current research regarding improving health-related QoL [24].
The alignment of the current study’s findings with the systematic review by Ughreja et al. is noteworthy. According to the meta-analysis outcomes, there was a notable decrease in pain after treatment and a moderate benefit that continued for another six months. In comparison to sham therapies, they concluded that there is moderate evidence in favor of the usefulness of myofascial release provided by a therapist and self-administered by individuals with FM syndrome in improving pain alleviation, sleep quality, and overall QoL [25].
Moreover, another systematic review was conducted to examine the scientific literature to gain an overview of the effectiveness of manual therapy in treating pain, mitigating the effects of the condition, and QoL in FM patients compared to controls or other treatments through randomized clinical trials. Myofascial release was the most frequently used intervention. Based on extremely low to moderate-quality evidence, the available data on manual therapy in patients with FM are insufficient to support and suggest its use in this population. However, osteopathy is the most effective among other manual therapy treatment options [26]. Various studies consider the myofascial release technique as a practical therapeutic choice, while others disagree with this statement.
In conclusion, various treatment alternatives exist for the management of FM. This study favors myofascial release therapy as a valuable complement to conventional physical therapy, offering the potential for improved outcomes when considering the comprehensive wellbeing of FM patients and going beyond just pain management. These nuanced results add to the ongoing discussion over the possible benefits of myofascial release techniques for treating FM.
Conclusion
The current study suggests that myofascial release therapy for the treatment of FM does not make any improvement in pain compared with passive stretching alone. However, the myofascial release technique is more advantageous in enhancing the QoL of FM patients, as evident from the FIQR findings. So, myofascial release technique can be used as an adjunct therapy for FM patients.
Study limitations
The sample size in the current study was small, limiting the generalizability of results. The extensive vocabulary of the MPQ might have affected the outcome of the results. Moreover, the duration of the treatment program used in this study could not describe the long-term effects.
Ethical Considerations
Compliance with ethical guidelines
The Ethical Review Committee of Riphah International University RCR & AHS/REC/MS-OMPT/027 approved the study.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Investigation: Sahar Aslam and Nida Ilahi; Writing the original draft: Sahar Aslam; Conceptualization, methodology, validation, formal analysis, data curation, review and editing: All authors; Supervision: Syed Shakil ur Rehman.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors sincerely thank the study participants and the administration of Shalamar Hospital for permitting us to gather our research data.
References
Fibromyalgia (FM) is a syndrome characterized by prolonged multifocal pain. It is associated with sleep instabilities, fatigue, and cognitive dysfunction. Common co-morbid conditions include anger and anxiety. It is the second most common rheumatologic disorder [1]. Though the precise cause of FM is unknown, aberrations of the nervous system concerning the processing of pain may explain the prolonged pain. Patients with FM express hyper-excitability and hyper-responsiveness of the centralized nervous system (central sensitization). Nociceptive provocations from muscular tissue may contribute to FM syndrome [2]. FM is common, with a prevalence of 2% in the general population [3]. Estimates of prevalence and female preponderance vary widely (0.4% to >11% and >90% to <61%, respectively) [4]. Some patients with FM also experience other symptoms like headache, migraine, abdominal pain, and irritable bowel syndrome [5]. In the general population, the prevalence of FM is ominously lower than in communities with certain ailments [6]. There is a weakened threshold to pain by nociceptive receptors, leading to an augmented reaction to mechanical stimulus, intervened by the magnification of CNS signaling. Widespread pain has been a clinical attribute of FM. It is described by an augmented sensitivity to pressure and light touch [7]. Family history of joint problems and working status are significant risk factors for FM [8]. People diagnosed with FM frequently encounter challenges related to their mental and cognitive wellbeing. Issues like disrupted sleep, memory issues, feelings of anxiety, and depression are commonly observed and can significantly affect their quality of life (QoL) [9]. Systemic lupus erythematosus-related variables accompany FM, including photosensitivity, oral ulcers, and secondary Sjögren’s [10]. FM is associated with a 1.54-fold increased risk for inflammatory bowel disease [11]. The severity of pain and deprived mental health status is associated with clinically diagnosed FM [12].
The pharmacological approach to FM treatment includes selective serotonin reuptake inhibitors, tricyclic anti-depressants, anti-epileptic drugs, serotonin-norepinephrine reuptake inhibitors, and muscle relaxants [13]. Moreover, aerobic exercise, education, improving sleep habits, and cognitive-behavioral therapy can be administered as fundamental treatments for addressing all symptoms. Mind-body exercises are advised as principal approaches for managing pain, fatigue, and sleep issues. Mindfulness is recognized as a primary treatment for depression and a supplementary treatment for other symptoms. Additionally, various interventions, such as music therapy, relaxation techniques, warm baths, and localized heat, are suggested as supplementary treatments, depending on the symptoms [14]. Nonsteroidal anti-inflammatory drugs like ibuprofen and diclofenac have not proved their effectiveness as standalone treatments [15]. Moreover, Physical activity, like exercise or leisure physical training, is essential in managing FM [16].
Millions of individuals throughout the world suffer from FM, with women making up the majority of cases. FM drastically lowers their QoL and strains the patient and the healthcare system. As a result, research into alternate therapy modalities is necessary. Despite common usage and popularity, these therapies have shown vague, incomplete, and conflicting results. The rationale of the current study was to investigate the effects of myofascial release therapy on pain and the QoL in patients diagnosed with FM, which will pave the way for more tailored, effective, and comprehensive treatment strategies in the management of FM.
Materials and Methods
Study design and participants
This quasi-experimental study was conducted at the Physiotherapy Department of Shalamar Hospital, Lahore, Pakistan, from January 2019 to July 2019. Twenty-eight male and female patients clinically diagnosed with FM, aged 25 to 45 years, were recruited to participate in this study. Study participants were carefully chosen through a non-probability convenience sampling technique, while the sample size was calculated based on the McGill pain scale of the previous study [17]. The level of confidence was set at 0.95(95%). The statistical power was set at 0.8. Each patient provided written informed consent. Patients meeting the inclusion criteria for this study were those who, during their initial assessment, had been afflicted with moderate to severe pain and reported experiencing activity limitation due to pain for a minimum of one day within the past month. The patients who had a fever, infection, hypotension, respiratory disorder, alteration in cutaneous integrity, and those who had received non-pharmacological therapies were excluded. After initial screening, those meeting predetermined inclusion criteria were divided into two groups.
Study interventions
All patients benefited from standard care, including patient education and passive stretching. Group A included 14 patients who received myofascial release technique for treatment in addition to passive stretching. Group B included 14 patients who received passive stretching alone. Written informed consent was taken from every participant. The treatment program included 12 sessions over 4 weeks, 3 sessions per week performed by an experienced physiotherapist. Each treatment session took 30 minutes. Passive stretching consisted of holding for 30 seconds during each repetition. The myofascial release technique consisted of local stretching of muscles that contained tender points, like erector spinae muscles, utilizing the cross-handed technique in the prone lying position. The strength of pressure was accustomed to the individual subjective feelings of the patient during the application of the technique [18]. After the final treatment session, post-intervention pain and QoL measurements were recorded.
The data were analyzed using SPSS, software, version 21. Statistical significance was established at P≤0.05. Using descriptive statistics, frequency tables, and bar charts were provided to show the summary of group measurements. The normality of the data was assessed by the Shapiro-Wilk test. Age, pain rating index, and total FM impact questionnaire scores were normally distributed (P>0.05), but values of present pain index (PPI) were not normally distributed (P<0.05). Parametric tests were applied to find the change between the groups for variables showing normal distribution. The independent t-test was used on the pain rating index (PRI) of the McGill pain questionnaire (MPQ) and the revised FM impact questionnaire (FIQR). The non-parametric test, the Mann-Whitney test, was used to determine the change between the groups for variables not normally distributed, such as the PPI of the McGill pain questionnaire.
Outcome measures
Pre- and post-intervention pain assessment was done using the McGill pain questionnaire, and QoL was assessed by employing FIQR. MPQ is a tool administrated by the interviewer. It can be used to evaluate the effectiveness and efficacy of interventions for pain and to assess pain qualitatively associated with distinct nociceptive conditions and neuropathic pain disorders. The pain is scored between 0 and 78, where 0 indicates no pain, while higher scores correspond to more severe pain intensity [19]. MPQ has been validated in different languages and is a valid and reliable tool for assessing musculoskeletal pain [20].
FIQR is a self‐reported questionnaire that assesses various elements of extensive FM. The psychometric evaluation of FIQR has shown its consistency and validity in the Japanese population with FM. The questionnaire comprises 21 items gauging three domains: “Function,” which included 9 items; “overall impact” of FM on functioning and severity of symptoms, consisting of two items; and “symptoms,” containing 10 items. Every item is scored on a numeric scoring scale with a score ranging from 0 to 10. The results of each domain are summed up, including the function, which ranges from 0 to 90. Overall impact ranges from 0 to 20, and symptoms vary from 0 to 100. After summing the results for every domain, the domains will be normalized by dividing by 3, 1, and 2, respectively. The overall FIQR score is calculated by three domain scores ranging from 0-100. A reduced score shows a better QoL [21].
Data analysis
Age, PRI, and total FM impact questionnaire scores were normally distributed (P>0.05), while values of PPI were not (P<0.05).
Results
A total of 28 subjects contributed to the study. They were equally divided into two groups. Selected subjects in one group were treated with myofascial release therapy and passive stretching, while the other group was treated with passive stretching alone.
The Mean±SD ages of groups A and B were 33.576.18 and 37.21±5.91 years, respectively.
The male-to-female ratio in group A was 6:8, while in group B, it was 5:9.
Table 1 shows that the Mean±SD pre-treatment score of the PRI in group A was 46.76±10.47, and in group B was 43.36±12.7.
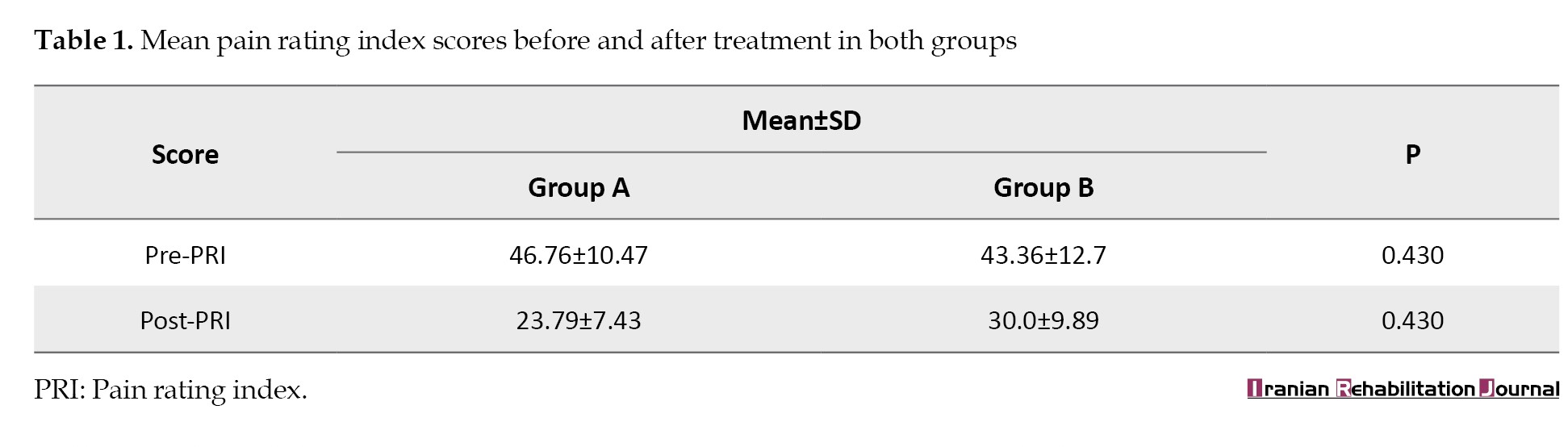
The Mean±SD of the post-treatment score of PRI in group A was 23.79±7.43, and in group B was 30.0±9.89. There was no significant difference in both groups for both pre- and post-PRI scores (P>0.05). Both groups showed equal improvement in PRI scores.
The A and B groups’ Mean±SD pre-treatment PPI scores were observed as 3.21±0.893 and 3.50±1.092 (Table 2).
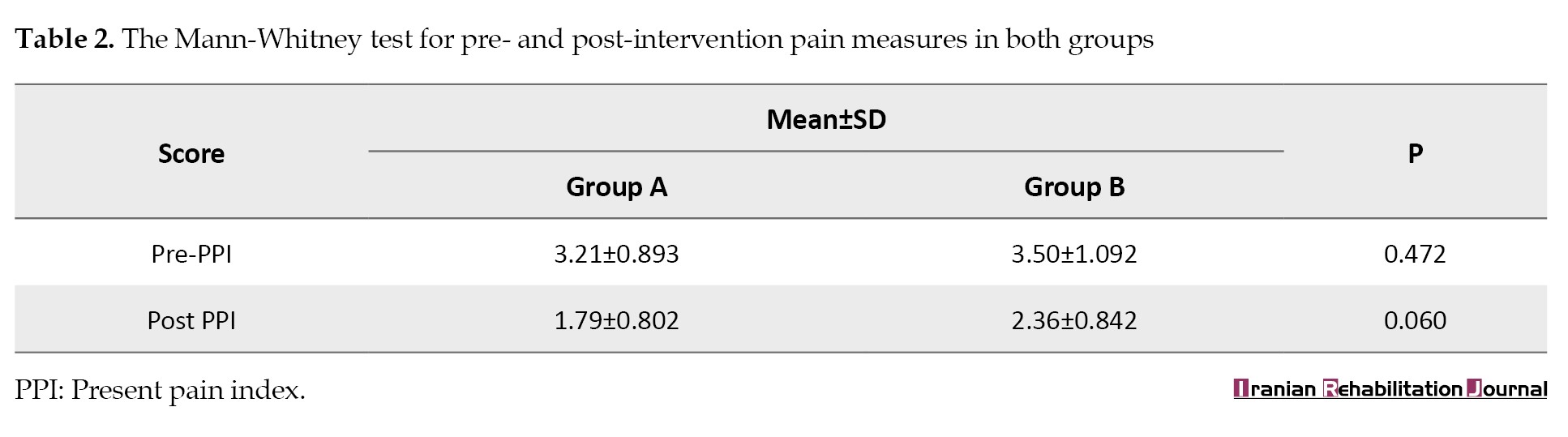
Also, Mean±SD post-treatment PPI scores in group A were 1.79±0.802, and in group B was 2.36±0.842 (P>0.05). In contrast, the difference in the mean scores of the two groups was not statistically significant. Similarly, there was no significant difference in both groups’ pre- and post-treatment scores (P>0.05). Both groups showed equal improvement in PPI scores (Table 2).
Moreover, the pre-treatment FIQR scores of both groups did not show any significant difference (P>0.05). However, when the mean FIQR scores of post-treatment of the two groups were compared, it revealed a significant difference (P<0.05). More improvement was noted in the FIQR score of group A than in group B (Table 3).
Discussion
The current study determines the effects of the myofascial release technique on pain and QoL in patients with clinically diagnosed FM.
After pre- and post-intervention analysis, there was an improvement in pain in both groups, but there was no significant difference between the groups in terms of pre- and post-scores. The QoL recorded on the FIQR was improved in both groups. However, the difference in the means of post-treatment scores of the two groups was significant, showing that more improvement was noted in the FIQR score of group A, who received myofascial release technique in addition to passive stretching, than in group B, who just received passive stretching.
Similarities with the current study’s findings were reported in an investigation that was intended to discover the advantages of applying self-myofascial release intervention on wellbeing-related to QoL in FM patients, and it concluded that the use of a self-myofascial release program improved the wellbeing life quality of individuals having FM [22].
Our study aligns with a single-blind, randomized controlled trial to compare the impacts of dry needling and myofascial release on FM patients. The study recommended that dry needling is more compelling than myofascial release in addressing pain in FM patients. They highlighted the potential of dry needling as a useful alternative for managing FM symptoms [2].
Similar to the current research findings, a systematic review by Laimi et al. about the efficacy of myofascial release therapy in treating persistent musculoskeletal pain revealed that myofascial release therapy is insufficient for chronic pain [23].
Moreover, varied results were demonstrated by a systematic review conducted by Yuan et al., aimed to evaluate the efficacy of different forms of soft tissue manipulation in treating FM. Compared to a placebo, the myofascial release showed significantly better pain results than the current study. However, similar trends were observed between that systematic review and the current research regarding improving health-related QoL [24].
The alignment of the current study’s findings with the systematic review by Ughreja et al. is noteworthy. According to the meta-analysis outcomes, there was a notable decrease in pain after treatment and a moderate benefit that continued for another six months. In comparison to sham therapies, they concluded that there is moderate evidence in favor of the usefulness of myofascial release provided by a therapist and self-administered by individuals with FM syndrome in improving pain alleviation, sleep quality, and overall QoL [25].
Moreover, another systematic review was conducted to examine the scientific literature to gain an overview of the effectiveness of manual therapy in treating pain, mitigating the effects of the condition, and QoL in FM patients compared to controls or other treatments through randomized clinical trials. Myofascial release was the most frequently used intervention. Based on extremely low to moderate-quality evidence, the available data on manual therapy in patients with FM are insufficient to support and suggest its use in this population. However, osteopathy is the most effective among other manual therapy treatment options [26]. Various studies consider the myofascial release technique as a practical therapeutic choice, while others disagree with this statement.
In conclusion, various treatment alternatives exist for the management of FM. This study favors myofascial release therapy as a valuable complement to conventional physical therapy, offering the potential for improved outcomes when considering the comprehensive wellbeing of FM patients and going beyond just pain management. These nuanced results add to the ongoing discussion over the possible benefits of myofascial release techniques for treating FM.
Conclusion
The current study suggests that myofascial release therapy for the treatment of FM does not make any improvement in pain compared with passive stretching alone. However, the myofascial release technique is more advantageous in enhancing the QoL of FM patients, as evident from the FIQR findings. So, myofascial release technique can be used as an adjunct therapy for FM patients.
Study limitations
The sample size in the current study was small, limiting the generalizability of results. The extensive vocabulary of the MPQ might have affected the outcome of the results. Moreover, the duration of the treatment program used in this study could not describe the long-term effects.
Ethical Considerations
Compliance with ethical guidelines
The Ethical Review Committee of Riphah International University RCR & AHS/REC/MS-OMPT/027 approved the study.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Investigation: Sahar Aslam and Nida Ilahi; Writing the original draft: Sahar Aslam; Conceptualization, methodology, validation, formal analysis, data curation, review and editing: All authors; Supervision: Syed Shakil ur Rehman.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors sincerely thank the study participants and the administration of Shalamar Hospital for permitting us to gather our research data.
References
- Siracusa R, Paola RD, Cuzzocrea S, Impellizzeri D. Fibromyalgia: Pathogenesis, mechanisms, diagnosis and treatment options update. International Journal of Molecular Sciences. 2021; 22(8):3891. [DOI:10.3390/ijms22083891]
- Castro Sánchez AM, García López H, Fernández Sánchez M, Pérez Mármol JM, Aguilar-Ferrándiz ME, Luque Suárez A, et al. Improvement in clinical outcomes after dry needling versus myofascial release on pain pressure thresholds, quality of life, fatigue, pain intensity, quality of sleep, anxiety, and depression in patients with fibromyalgia syndrome. Disability and Rehabilitation. 2019; 41(19):2235-46. [DOI:10.1080/09638288.2018.1461259] [PMID]
- Ożóg P, Weber-Rajek M, Radzimińska A, Goch A. Analysis of postural stability following the application of myofascial release techniques for low back pain-a randomized-controlled trial. International Journal of Environmental Research and Public Health. 2023; 20(3):2198. [DOI:10.3390/ijerph20032198]
- Wolfe F, Walitt B, Perrot S, Rasker JJ, Häuser W. Fibromyalgia diagnosis and biased assessment: Sex, prevalence and bias. PloS One. 2018; 13(9):e0203755. [PMID]
- Häuser W, Sarzi-Puttini P, Fitzcharles MA. Fibromyalgia syndrome: Under-, over-and misdiagnosis. Clinical and Experimental Rheumatology. 2019; 37(Suppl 116):90-7. [PMID]
- Kleinstäuber M. Somatic symptom and related disorders. In: IsHak WW, editor. Atlas of psychiatry. Cham: Springer; 2023.[DOI:10.1007/978-3-031-15401-0_20]
- Augière T, Desjardins A, Paquette Raynard E, Brun C, Pinard AM, Simoneau M, et al. Tactile detection in fibromyalgia: A systematic review and a meta-analysis. Frontiers in Pain Research. 2021; 2:740897. [DOI:10.3389/fpain.2021.740897] [PMID]
- Tan AC, Jaaniste T, Champion D. Chronic widespread pain and fibromyalgia syndrome: Life-course risk markers in young people. Pain Research and Management. 2019; 2019:6584753. [DOI:10.1155/2019/6584753] [PMID]
- Kaleycheva N, Cullen AE, Evans R, Harris T, Nicholson T, Chalder T. The role of lifetime stressors in adult fibromyalgia: systematic review and meta-analysis of case-control studies. Psychological Medicine. 2021; 51(2):177-93. [DOI:10.1017/S0033291720004547]
- Fung W, Touma Z. Consideration of fibromyalgia in the assessment and treatment of SLE. Current Treatment Options in Rheumatology. 2021; 7(3):182-93. [DOI:10.1007/s40674-021-00181-2]
- Singh L, Kaur A, Bhatti MS, Bhatti R. Possible molecular mediators involved and mechanistic insight into fibromyalgia and associated co-morbidities. Neurochemical Research. 2019; 44:1517-32. [DOI:10.1007/s11064-019-02805-5]
- Sarzi-Puttini P, Giorgi V, Marotto D, Atzeni F. Fibromyalgia: An update on clinical characteristics, aetiopathogenesis and treatment. Nature Reviews Rheumatology. 2020; 16(11):645-60. [DOI:10.1038/s41584-020-00506-w] [PMID]
- El-Tallawy SN, Nalamasu R, Salem GI, LeQuang JAK, Pergolizzi JV, Christo PJ. Management of musculoskeletal pain: An update with emphasis on chronic musculoskeletal pain. Pain and Therapy. 2021; 10:181-209. [DOI:10.1007/s40122-021-00235-2] [PMID]
- Kundakci B, Hall M, Atzeni F, Branco J, Buskila D, Clauw D, et al. International, multidisciplinary Delphi consensus recommendations on non-pharmacological interventions for fibromyalgia. Seminars in Arthritis and Rheumatism. 2022; 57:152101. [DOI:10.1016/j.semarthrit.2022.152101]
- Rico-Villademoros F, Postigo-Martin P, Garcia-Leiva JM, Ordoñez-Carrasco JL, Calandre EP. Patterns of pharmacologic and non-pharmacologic treatment, treatment satisfaction and perceived tolerability in patients with fibromyalgia: A patients’ survey. Clinical and Experimental Rheumatology. 2020; 38(Suppl 123):72-8. [PMID]
- Bidonde J, Boden C, Foulds H, Kim SY. Physical activity and exercise training for adults with fibromyalgia.In: Ablin JN, Shoenfeld Y, editors. Fibromyalgia Syndrome. Cham: Springer; 2021. [DOI:10.1007/978-3-030-78638-0_6]
- Castro-Sánchez AM, Matarán-Penarrocha GA, Arroyo-Morales M, Saavedra-Hernández M, Fernández-Sola C, Moreno-Lorenzo C. Effects of myofascial release techniques on pain, physical function, and postural stability in patients with fibromyalgia: A randomized controlled trial. Clinical Rehabilitation. 2011; 25(9):800-13. [DOI:10.1177/0269215511399476]
- Dhiman, Neetu Rani et al. Myofascial release versus other soft tissue release techniques along superficial back line structures for improving flexibility in asymptomatic adults: A Systematic review with meta-analysis. Journal of Bodywork and Movement Therapies. 2021; 28,450-7. [DOI: 10.1016/j.jbmt.2021.06.026] [PMID]
- Katz J, Melzack R. McGill Pain Questionnaire. In: Maggino F, editor. Encyclopedia of quality of life and well-being research. Cham: Springer. [DOI:10.1007/978-3-319-69909-7_1748-2]
- Leme OP, Yuan S, Magalhães MO, de Meneses SF, Marques AP. Pain and quality of life in knee osteoarthritis, chronic low back pain and fibromyalgia: A comparative cross-sectional study. Reumatismo - The Italian Journal of Rheumatology. 2019; 71(2):68-74. [DOI:10.4081/reumatismo.2019.1104]
- Isomura T, Nakamura I, Kawaguchi M, Sato E, Inuzuka K, Osada K, et al. Psychometric assessment of the Japanese version of the Revised Fibromyalgia Impact Questionnaire: Reliability and validity. International Journal of Rheumatic Diseases. 2017; 20(9):1088-94. [DOI:10.1111/1756-185X.12574]
- Ceca D, Elvira L, Guzman JF, Pablos A. Benefits of a self-myofascial release program on health-related quality of life in people with fibromyalgia: A randomized controlled trial. The Journal of Sports Medicine and Physical Fitness. 2017; 57(7-8):993-1002. [DOI:10.23736/S0022-4707.17.07025-6]
- Laimi K, Mäkilä A, Bärlund E, Katajapuu N, Oksanen A, Seikkula V, et al. Effectiveness of myofascial release in treatment of chronic musculoskeletal pain: A systematic review. Clinical Rehabilitation. 2018; 32(4):440-50. [DOI:10.1177/0269215517732820] [PMID]
- Yuan SL, Matsutani LA, Marques AP. Effectiveness of different styles of massage therapy in fibromyalgia: A systematic review and meta-analysis. Manual Therapy. 2015; 20(2):257-64. [DOI:10.1016/j.math.2014.09.003] [PMID]
- Ughreja RA, Venkatesan P, Gopalakrishna DB, Singh YP. Effectiveness of myofascial release on pain, sleep, and quality of life in patients with fibromyalgia syndrome: A systematic review. Complementary Therapies in Clinical Practice. 2021; 45:101477. [DOI:10.1016/j.ctcp.2021.101477] [PMID]
- Schulze NB, Salemi MM, de Alencar GG, Moreira MC, de Siqueira GR. Efficacy of manual therapy on pain, impact of disease, and quality of life in the treatment of fibromyalgia: A systematic review. Pain Physician. 2020; 23(5):461-7. [PMID]
Article type: Original Research Articles |
Subject:
Physiotherapy
Received: 2023/09/11 | Accepted: 2024/01/28 | Published: 2024/12/20
Received: 2023/09/11 | Accepted: 2024/01/28 | Published: 2024/12/20
Send email to the article author








