Volume 22, Issue 1 (March 2024)
Iranian Rehabilitation Journal 2024, 22(1): 1-14 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Bahramizadeh M, Khaliliyan H, Sharafatvaziri A, Sadeghi-Demneh E, Szarpak L, Pruc M, et al . Postural Control Measures After Lateral Ankle Sprain While Wearing Ankle Orthoses: A Systematic Review. Iranian Rehabilitation Journal 2024; 22 (1) :1-14
URL: http://irj.uswr.ac.ir/article-1-2169-en.html
URL: http://irj.uswr.ac.ir/article-1-2169-en.html
Mahmood Bahramizadeh1 

 , Hanieh Khaliliyan *2
, Hanieh Khaliliyan *2 

 , Arash Sharafatvaziri3
, Arash Sharafatvaziri3 

 , Ebrahim Sadeghi-Demneh4
, Ebrahim Sadeghi-Demneh4 

 , Lukasz Szarpak5
, Lukasz Szarpak5 

 , Michal Pruc5
, Michal Pruc5 

 , Aanuoluwapo Adeyimika Afolabi6
, Aanuoluwapo Adeyimika Afolabi6 

 , Francesco Chirico7
, Francesco Chirico7 




 , Hanieh Khaliliyan *2
, Hanieh Khaliliyan *2 

 , Arash Sharafatvaziri3
, Arash Sharafatvaziri3 

 , Ebrahim Sadeghi-Demneh4
, Ebrahim Sadeghi-Demneh4 

 , Lukasz Szarpak5
, Lukasz Szarpak5 

 , Michal Pruc5
, Michal Pruc5 

 , Aanuoluwapo Adeyimika Afolabi6
, Aanuoluwapo Adeyimika Afolabi6 

 , Francesco Chirico7
, Francesco Chirico7 


1- Department of Orthotics and Prosthetics, School of Rehabilitation Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
2- Department of Orthotics and Prosthetics, School of Rehabilitation Sciences, Isfahan University of Medical Sciences, Isfahan, Iran.
3- Center for Orthopedic Trans-Disciplinary Applied Research, Tehran University of Medical Sciences, Tehran, Iran.
4- Musculoskeletal Research Center, Isfahan University of Medical Sciences, Isfahan, Iran.
5- Department of Clinical Research and Development, LUXMED Group, Warsaw, Poland.
6- Technical Services Directorate, MSI Nigeria Reproductive Choices, Abuja, Nigeria.
7- Post-graduate School of Occupational Health, Universita Cattolica del Sacro Cuore, Rome, Italy.
2- Department of Orthotics and Prosthetics, School of Rehabilitation Sciences, Isfahan University of Medical Sciences, Isfahan, Iran.
3- Center for Orthopedic Trans-Disciplinary Applied Research, Tehran University of Medical Sciences, Tehran, Iran.
4- Musculoskeletal Research Center, Isfahan University of Medical Sciences, Isfahan, Iran.
5- Department of Clinical Research and Development, LUXMED Group, Warsaw, Poland.
6- Technical Services Directorate, MSI Nigeria Reproductive Choices, Abuja, Nigeria.
7- Post-graduate School of Occupational Health, Universita Cattolica del Sacro Cuore, Rome, Italy.
Full-Text [PDF 715 kb]
(1290 Downloads)
| Abstract (HTML) (3596 Views)
Full-Text: (611 Views)
Introduction
Background of the population
Epidemiological research has indicated that lateral ankle sprains (LAS) are among the most frequent lower limb injuries in physically active individuals [1]. A sprain occurs when a ligament undergoes significant force or strain. The most common mechanism of this injury is a combination of plantarflexion and inversion movements with high velocity and torque [2]. Patients who have experienced an acute LAS are five times more likely to experience a repeat sprain [3], and over 40% of these individuals subsequently suffer from chronic ankle instability (CAI) [4, 5]. Researchers believe that CAI-related disorders originate from the primary damage that occurs during the initial sprain [6]. Patients with a history of significant LAS, recurrent sprains, episodes of ankle giving way, sensations of instability, or a decline in ankle function that persists for over a year may exhibit evidence of this condition [7, 8]. Long-term consequences, like ankle joint osteoarthritis, have been reported for individuals suffering from this condition [9]. Hiller et al. proposed a model for CAI, in which affected individuals are classified into three subgroups: Functional ankle instability (FAI), mechanical ankle instability (MAI), and repeated sprains [10]. MAI results in an expansion of the joint range of motion beyond the normal physiological level. It manifests as excessive inversion laxity of the rearfoot or excessive anterior laxity of the talocrural joint [11]. Functional instability in individuals with sprained ankles is due to disturbances in proprioceptive sense [12], skin sense [13-15], speed of nerve conduction [16], and neuromuscular response [12]. Damage to mechanoreceptors and nerve endings in the capsule, ligament, and ankle joint causes such instability [17].
Therefore, after the initial injury, different changes and defects occur at different levels of the neuromuscular system of the ankle and foot complex, and the multi-jointed nature of the complex as the base of the kinetic chain of the body causes more complications. Changes in CAI lead to extensive disorders, such as altered osteokinematics and muscle activity [18], which result in a change in postural control [12].
Ankle orthoses (AOs) and their effects
Due to the high prevalence of LAS and the large number of people who report subsequent CAI, it is necessary to manage the injury with rehabilitation interventions to compensate for or correct the disorders related to this complication. The usual treatment methods used are physiotherapy exercises [19], taping [20], and orthoses [21]. Most people prefer to use orthoses because doing physiotherapy exercises is time-consuming, and the tapes lose their effect after 10-40 minutes [22].
One of the most common clinical management approaches to acute and chronic ankle sprains is using AOs. It has been shown that these orthoses prevent primary and repeated injuries to the lateral ligaments and are usually used in CAI to increase the stability of the ankle joint. Using AOs leads to a 70% reduction in acute sprains among people with previous injuries and a 57% reduction among high school athletes without ankle injuries [23, 24]. Although the exact mechanism of injury prevention during orthosis use is unknown, the most prominent explanation involves sensory and mechanical effects. The mechanical effects are restriction of ankle and foot complex movements, while the sensory effects are caused by skin and mechanoreceptor stimulation, leading to proprioception improvement [25, 26].
Rationale
There have been several systematic reviews on the effectiveness of therapeutic interventions for LAS, indicating a high interest among researchers in finding the optimal treatment for this complication [27]. The effects of AOs on ankle biomechanics during changing directions, running, and landing have been investigated in two systematic studies [28, 29]. The first study looked at the effects of AOs on ankle biomechanics during a change of direction [28], while the second investigated the effects of AOs on peroneus longus muscle activity during sudden inversion in people with an ankle sprain [29]. However, the impact of AOs on postural control in individuals with acute, chronic, and functional LAS remains unclear. This systematic review aimed to determine whether AOs improve postural control in subjects with LAS.
Materials and Methods
Search method
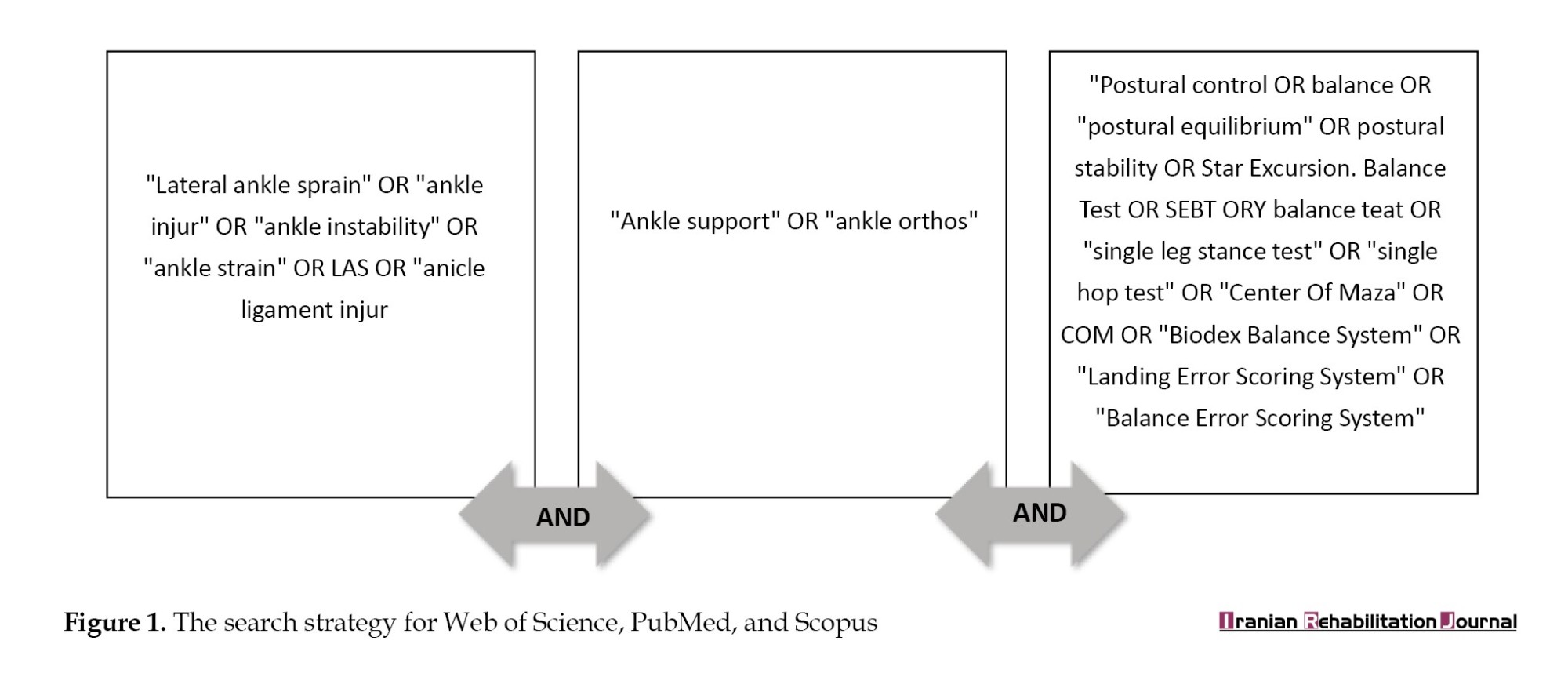
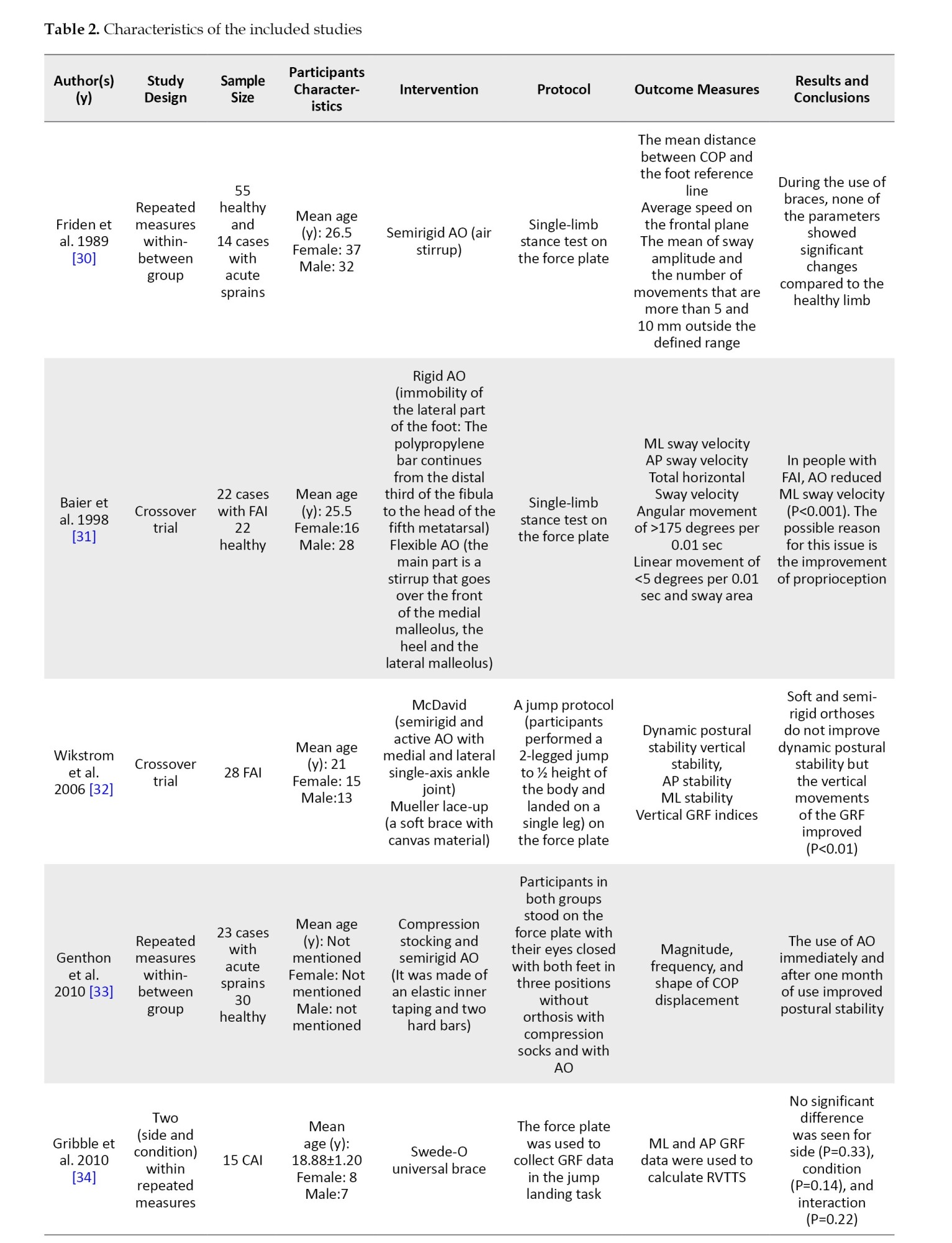
To conduct the search, relevant keywords were chosen, and their synonyms were identified through the MeSH database. Then, following the population, intervention, comparison, outcome measure (PICO) protocol and using Boolean logical operators, a search term was created (Figure 1). In May 2023, a systematic search was carried out using the search term on PubMed, Web of Science, and Scopus databases. The search scope was limited to titles, keywords, and abstracts across all databases.
Eligibility criteria and selection process
This systematic study was done based on the PRISMA flow diagram. After the initial search, the title, keywords, and abstract of all the articles in English indexed in the reputable journals listed in the three databases were entered into the Endnote software, version 20.5.0. All these articles were published after peer review. The selection of articles was done by following the process mentioned below:
1) All duplicate articles were removed.
2) The title, keywords, and abstract were reviewed by three researchers based on the following criteria:
Inclusion criteria:
• Patients were individuals with acute, functional, or chronic LAS.
• The intervention used included various types of AOs.
• The outcome measures included all the variables that can be attributed to postural control based on the available documentation.
• Comparing the effects of the intervention on a group of individuals with CAI, FAI, and acute LAS with a control group, or with the contralateral healthy leg or with pre-intervention conditions.
Exclusion criteria:
• The studied population had sprains caused by musculoskeletal disorders or comorbidities such as ligament laxity.
• Patients received other conservative interventions such as physical therapy or non-steroidal anti-inflammatory drugs.
• Articles published as letters to the editor and commentary.
• Articles that studied animals.
3) The full texts of the included articles were obtained. Then, by reviewing the references of the articles, other articles deemed suitable were also retrieved.
4) The full texts of these articles were screened again by three reviewers according to the predefined inclusion criteria.
In cases where there was a disagreement between three authors on enlisting an article, other authors made the final decision.
Assessing the quality of articles
The studies included in this systematic review were rated as level 2 or higher according to the National Health and Medical Research Council (NHMRC). The selected papers were assessed using the physiotherapy evidence database (PEDro) scale, which consists of 11 criteria. Each criterion is answered with a yes or no, with a score of one assigned for yes answers and zero for no answers. The final score was calculated between 1 and 10 without considering the first item. Methodological quality was determined as follows: Studies scoring 0-4 were considered poor, 4-5 were fair, 6-8 were good, and studies scoring 9-10 were excellent.
Data extraction, presentation, and analysis
Information was extracted from each included trial on: 1) Characteristics of the trial (mean age, gender, history of acute LAS/FAI/CAI) and control group (healthy group, randomized allocation, or without control group) participants; 2) Type and characteristics of AOs; 3) Type of outcome measures (COP parameters, clinical tests, and indices related to dynamic postural control). Also, the information related to study design, assessment protocol, and final conclusions were collected from the studies. There was no data pooling or meta-analysis because the included studies did not all use the -same protocols, assessment tools, foot condition (barefoot or wearing shoes), or definition of LAS (acute, functional, or chronic).
Results
Study selection
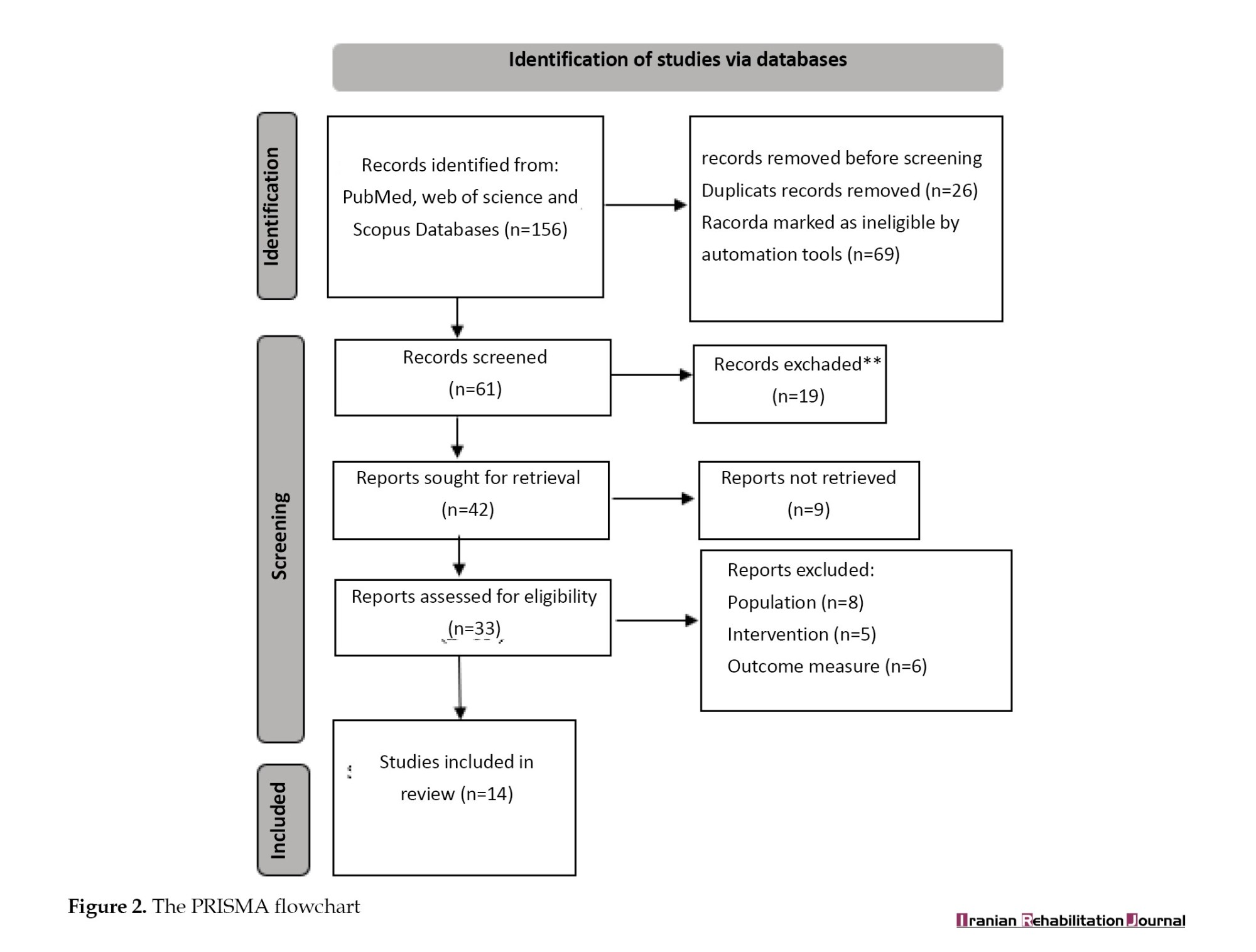
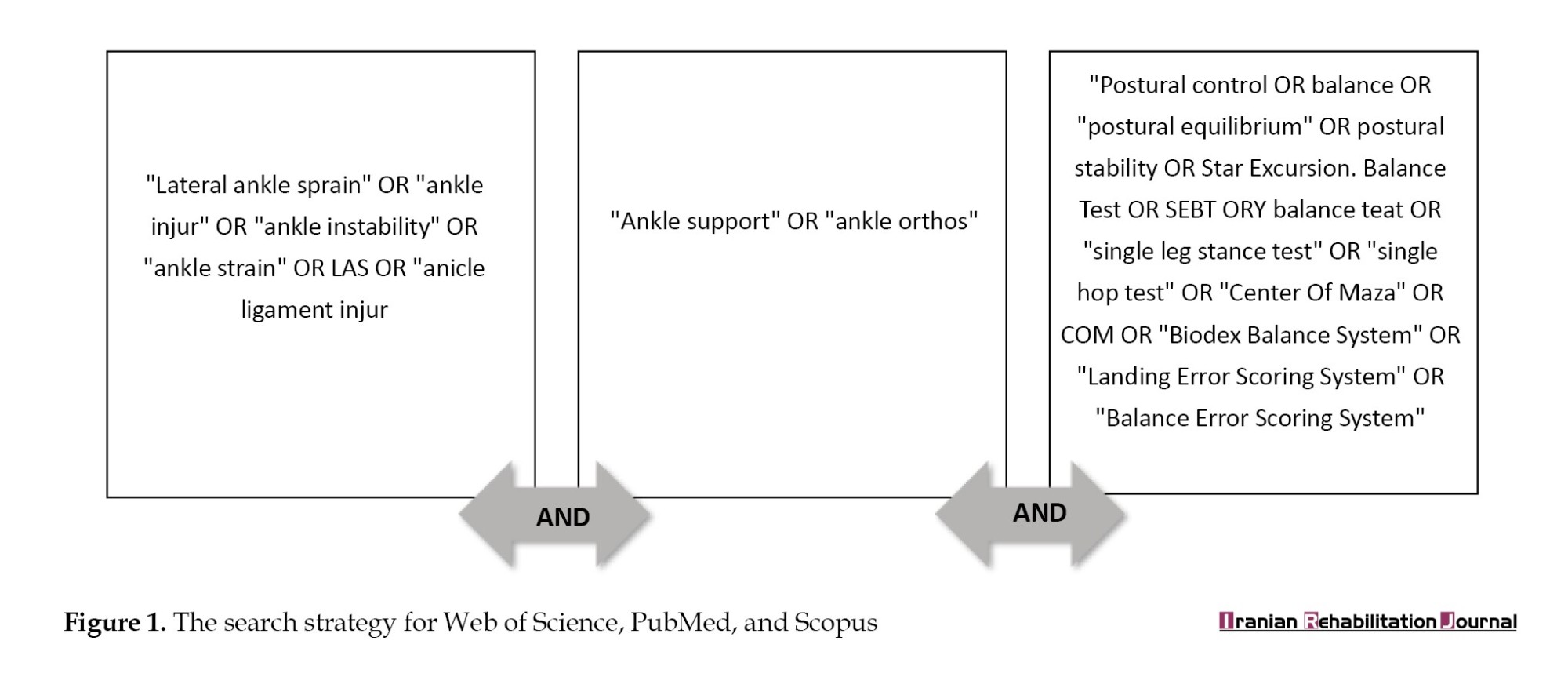
After conducting the initial search, we found 156 articles. However, after following the steps outlined in the PRISMA flowchart, only 14 articles met the necessary criteria for this study (Figure 2).
Methodological quality assessment
After examining the level of studies according to the NHMRC classification, two studies were at level 2 (having at least one properly designed RCT) [38, 42], and the rest were at level 3 (controlled trial without randomization).
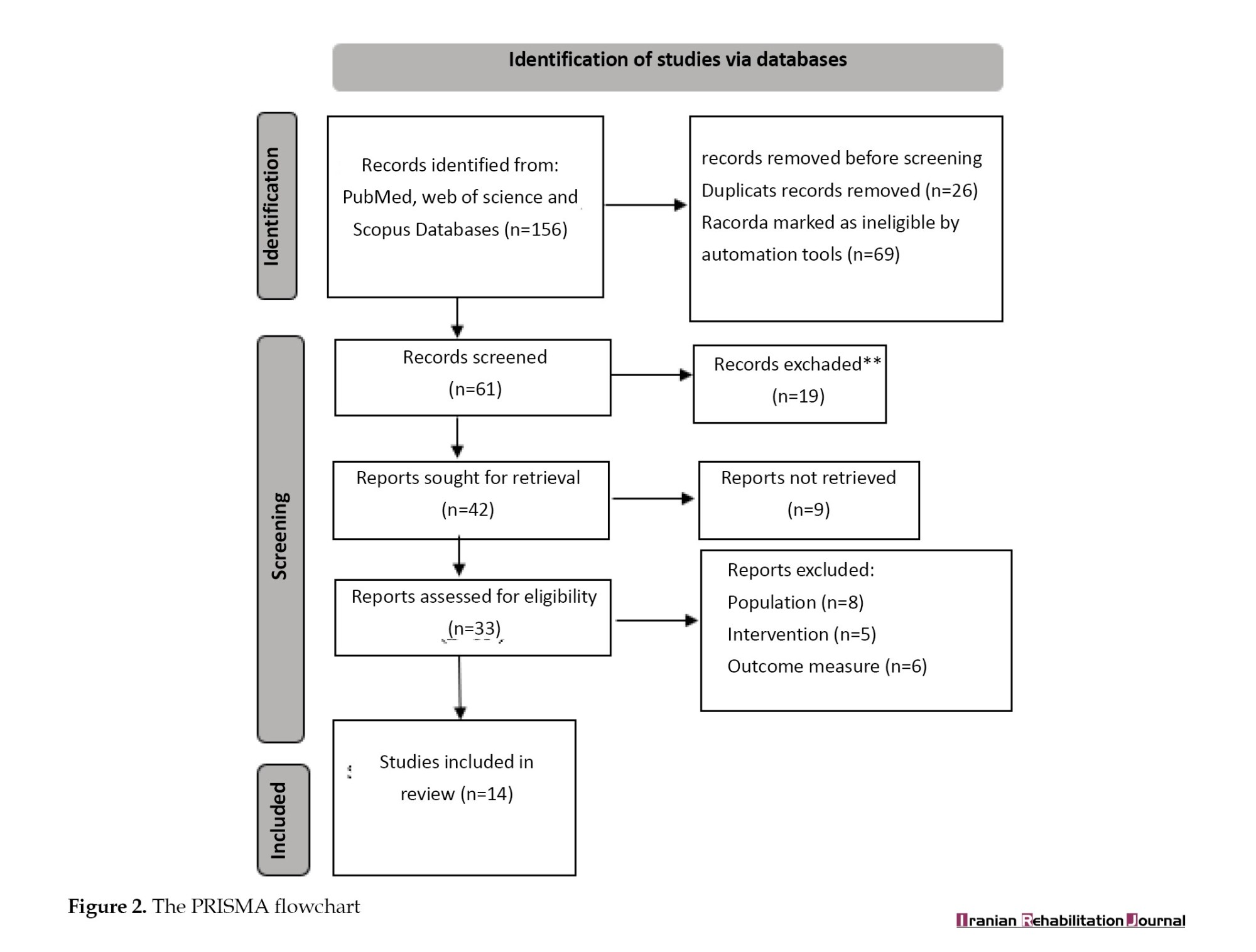
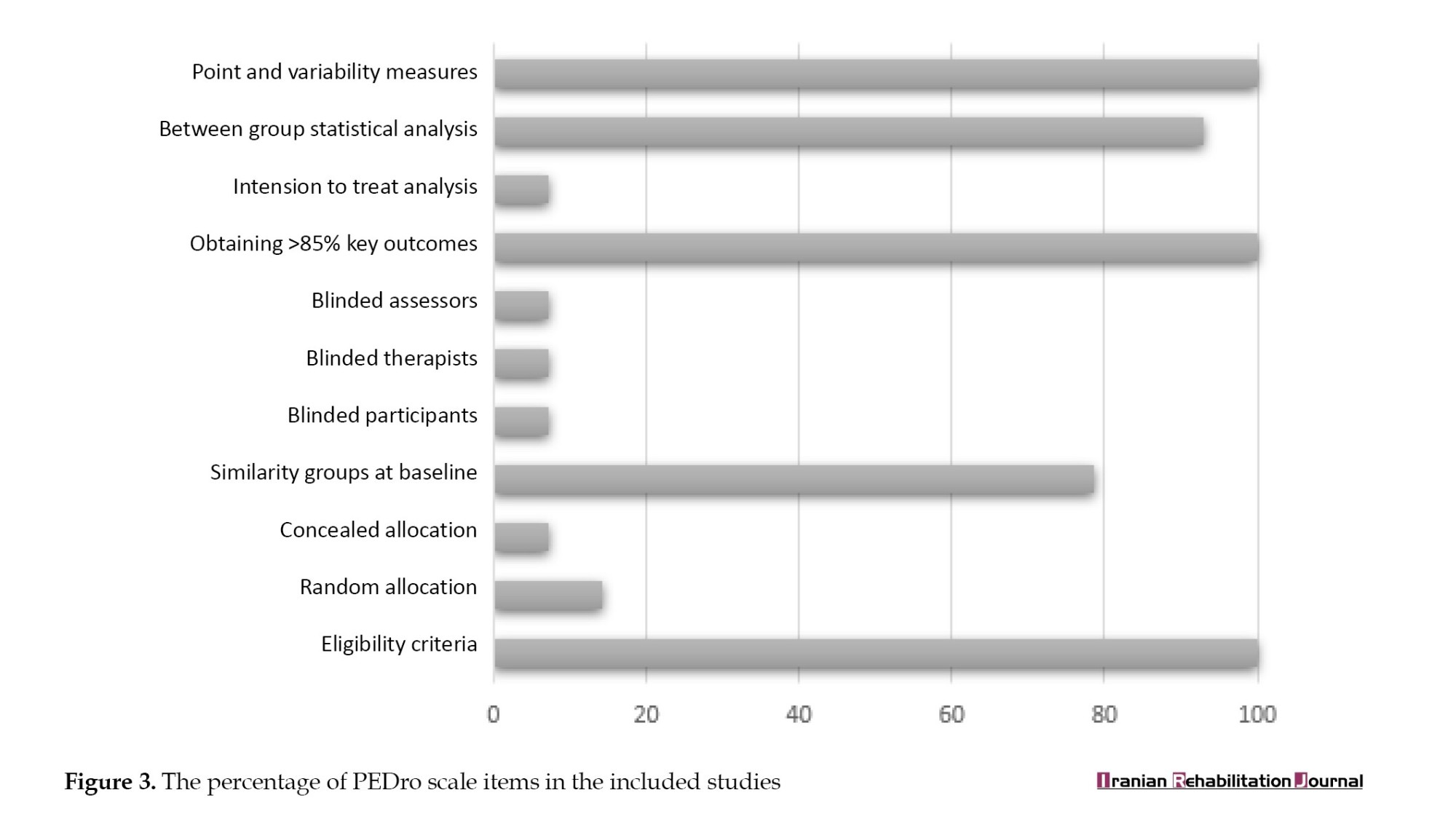
In this study, the quality of the methodology was evaluated using PEDro’s scale (Table 1).
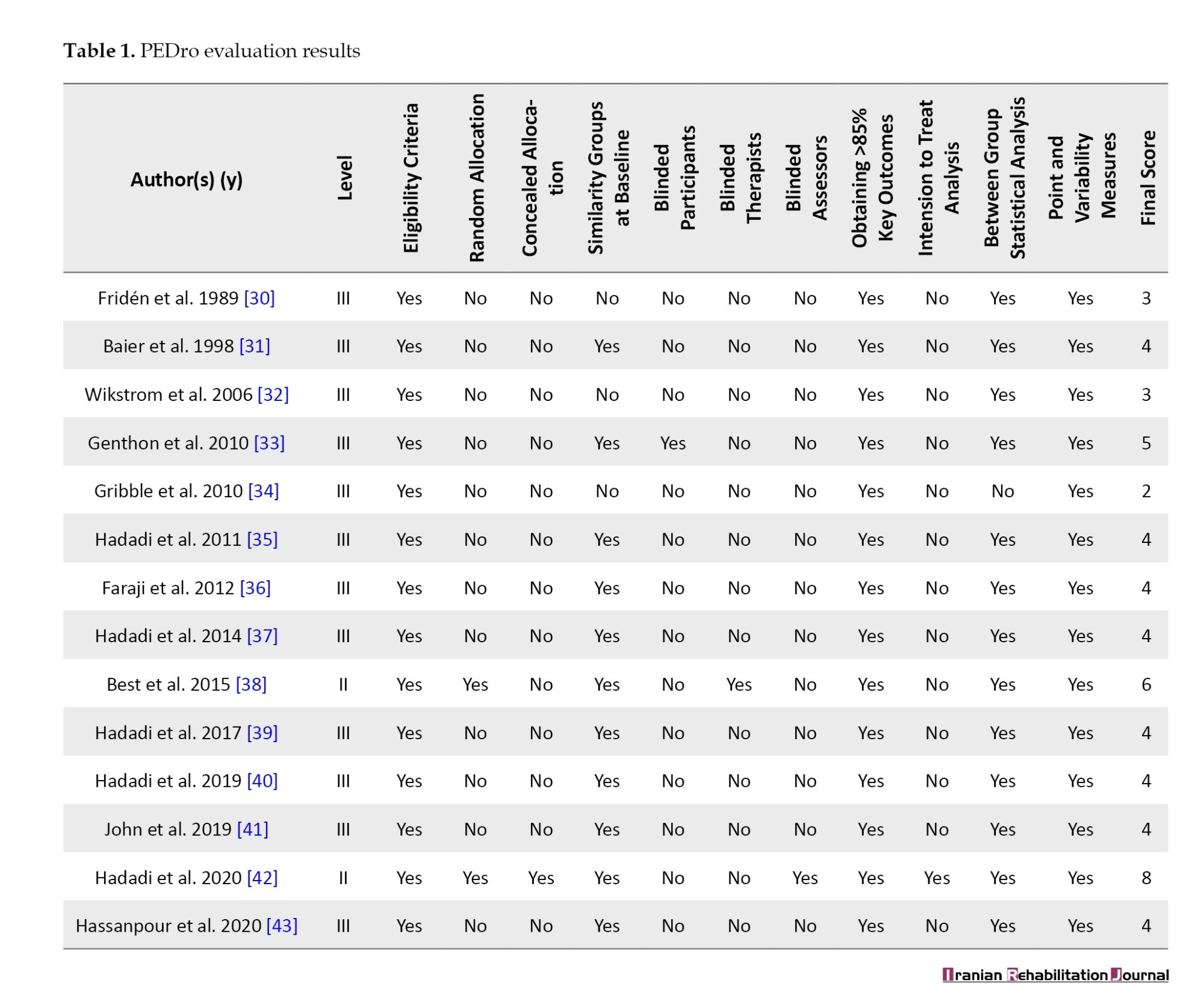
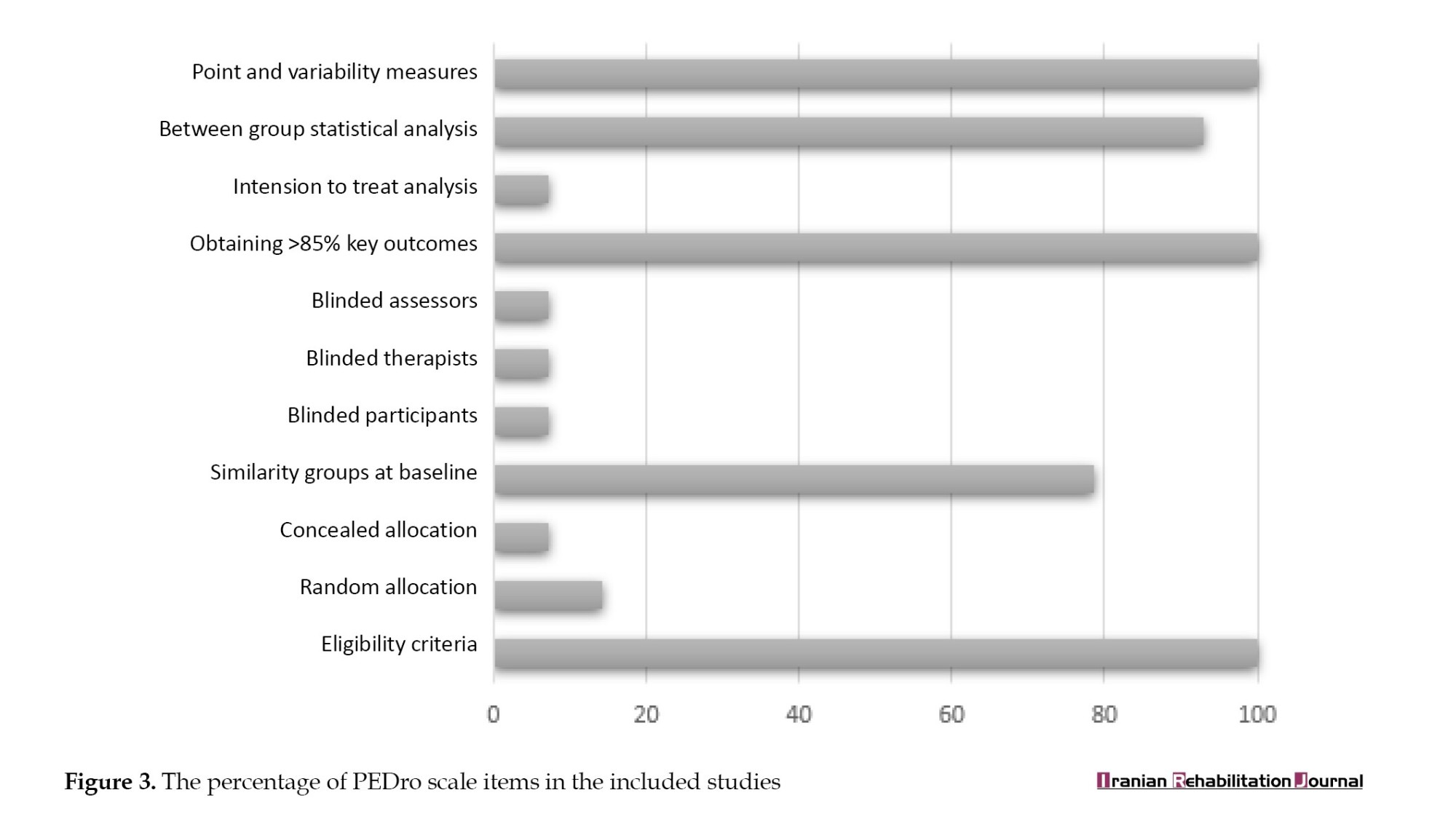
Results showed that all studies had identified eligibility criteria, obtained results from more than 85% of participants, and reported diversity criteria. However, the risk of bias in the studies was very high regarding randomization and blinding. Furthermore, only one of the studies, which was an RCT, explained the attrition rate and its cause. Figure 3 displays the overall results of PEDro’s checklist items as percentages.
Study characteristics
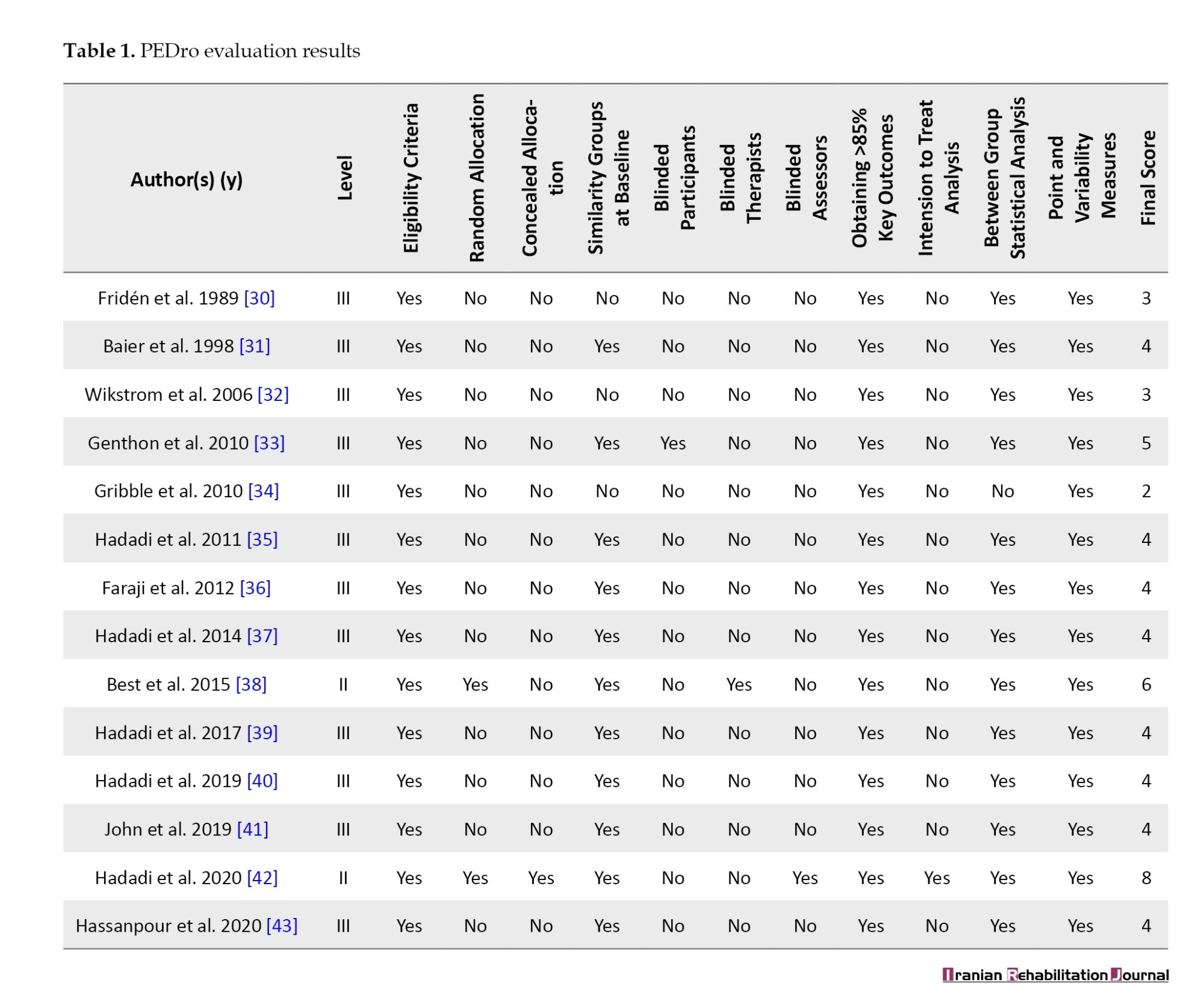
The text below presents the search results from the articles included in this study, categorized based on the characteristics of the samples, interventions, and outcomes. The study’s features are outlined in Table 2.


Participant’s characteristics
The studies involved a total of 678 participants, of whom 96 had acute sprains, 86 had FAI, and 172 had CAI. Additionally, 324 healthy individuals were included as part of the control group. The size of each sample varied from 15 to 124, with a mean of 45 people per study. The overall mean age of the participants was 23.4 years, except for one study where the mean age of the samples was not reported.
Interventions
Different terms were used to describe the types of AOs. Generally, AOs used in studies were divided into two types: Customized and prefabricated. In 12 studies, prefabricated AOs were used, while in two studies, customized types were used. Customized AOs were made according to the size of the individual’s foot and ankle complex, which was composed of a combination of a soft ankle sleeve, footplate, and ML stirrup support [39, 40].
The most common method of categorizing prefabricated AOs was based on the hardness of the materials used. Accordingly, AOs were divided into three categories: Rigid, semi-rigid, and soft. The rigid type had a hard lateral section of polyethylene that originated from the distal third of the fibula and terminated at the head of the 5th metatarsal. This orthosis aims to significantly reduce inversion, eversion, plantarflexion, and dorsiflexion movements [30, 38]. The semi-rigid type is typically made of a layer of neoprene [36, 40], canvas [37, 39], nylon [35, 44], and two-sided bars or U-shaped stirrups [37-39]. Additionally, in the active AO, which is considered a semi-rigid type, there are single-axis joints at each side of the ankle [36, 40-42], resulting from the connection of U-shaped stirrups with the lateral bars. Semi-rigid AOs allow movement in the sagittal plane while preventing inversion and eversion [37]. The soft type is usually made of a layer of neoprene [36], nylon [37, 39, 42], or canvas [30-32] and may have a double-sided spring [35, 37, 39] for relative lateral and medial support. The purpose of making soft AOs is to provide support and slightly reduce the movements of the ankle joint at the end of the ankle’s range of motion in different planes [44]. To secure these orthoses on the ankle, various fastening methods (circumferential [43], figure-of-eight [32, 39, 40], triple-stitched straps [42], and lace-up [30, 31] were used.
Outcomes
In this section, we categorized the different variables that the researchers measured and associated with the concept of postural control.
COP parameters
In three studies [35, 39, 40], the Mean±SD total velocity in anteroposterior (AP) direction, SD of velocity in mediolateral (ML) direction, phase plane portrait, phase plane portrait AP, and phase plane portrait ML were used as parameters for measuring static postural control. The impact of soft, semirigid, and combined mechanism ankle support (CMAS) orthoses on these parameters was assessed, and it was found that there were significant improvements in the phase plane portrait (F(2, 38)=4.32, P=0.03), mean total velocity (F(2, 38)=4.60, P=0.02) [35], and all COP parameters (P˂0.02) [39], respectively. Furthermore, the results of a post hoc test indicated that CMAS had a significant decrease in all COP parameters (P˂0.05) compared to soft AO and foot orthoses (FO) [40].
In two studies [30, 31], different COP parameters were used to check postural control. These included sway area, ML sway velocity, AP sway velocity, total horizontal sway velocity, angular movement of >175 degrees per 0.01 sec, and lineal movement of <5 degrees per 0.01 sec. Soft (P˂0.001) and semi-rigid (P=0.002) AOs in the FAI group significantly affected ML sway velocity. The soft orthosis significantly reduced lineal movement by <5 degrees per 0.01 sec (P=0.002) [31].
Genthon et al. [33] considered magnitude, frequency, and displacement shape as COP parameters. They found that the shape of displacement (P˂0.05) and magnitude (P˂0.001) in the semirigid AO group were significantly lower than those in the compression stockings and no orthosis groups.
Best et al. [38] used the sum of frontal and sagittal COP movements in each time unit to obtain the total oscillation distance. This method found no difference between rigid and semirigid orthoses in improving postural control.
Clinical tests
In five studies [37, 40-43] the star excursion balance test (SEBT) was used to evaluate dynamic postural control. The comparison of soft and semirigid orthoses showed a significant increase in distance difference in the posteromedial (5% difference, P˂0.05) [37], anterior (0.048), and anterolateral (P=0.046) directions when using the soft one [43]. When comparing CMAS with soft AO and FO, it was observed that the reaching distance increased in the medial direction (P=0.022 in the comparison between FO and CMAS) and anteromedial direction (P=0.046 in the comparison between FO and CMAS, and P=0.042 in the comparison between soft AO and CMAS) when CMAS was utilized [40]. However, a study by John et al. [41] found that soft AO had no impact on the Y balance test [41].
In a study [42], the single leg stance test (SLST) was used to evaluate static postural control. The results revealed no significant differences in the use of soft, semi-rigid AOs, or Kinesio tape. Additionally, the same study utilized the Single Hop Test and Y balance test to evaluate dynamic postural control, and the findings indicated that the measured distance did not significantly differ when using soft, semi-rigid AOs, or Kinesio tape.
Indexes related to dynamic postural control
Some of the indices used to compare control, soft AOs, and semi-rigid AOs were vertical stability, AP stability, ML stability, and dynamic postural stability. The results showed that the use of soft and semi-rigid AOs led to a significant improvement in the vertical GRF index (P<0.01) [32]. When using the Biodex device, it was found that both soft and semi-rigid AOs significantly improved the dynamic (F=5.1, P=0.01) and semi-dynamic (F=6.2, P<0.001) indices compared to the group without orthosis [36].
Hassanpour et al. compared soft and semi-rigid AOs by calculating AP stability, ML stability, and overall stability indices and found no difference between the two groups [43]. In another study, Gribble et al. calculated the resultant vector time to stabilization (RVTTS) index using AP and ML GRF data. The researchers discovered that using an AO did not significantly affect this index [34]. Additionally, the use of elastic AOs in individuals with CAI did not result in improved performance on the landing error scoring system (LESS) or balance error scoring system (BESS) [41].
Discussion
The recovery of postural control is the foundation of rehabilitation following LAS [44]. AOs are frequently utilized in sports to enhance postural control, and they are widely accepted and utilized due to their ease of use, adjustability, and reasonable price [45]. AOs are complex biomechanical interventions that vary in terms of materials, fastening methods, and their ability to create stability [46].
Static postural control
Some studies found AOs to be effective in improving static postural control in subjects with LAS [30, 31, 35, 39, 40, 42], but John et al. said that elastic AO was not effective in improving static or dynamic postural control [41]. One possible explanation for the conflicting results may be the reliability of the BESS used in Johns et al.’s study [41]. Finnoff et al. reported that the inter-rater reliability of BESS is poor [47]. Additionally, Best et al. believe that semirigid AOs are not effective in improving postural control after LAS. They investigated the effect of this orthosis on postural control in individuals with acute sprains and obtained conflicting results compared to those with chronic or functional sprains [38].
Based on research findings, AOs are effective in improving static postural control. After an ankle sprain, the range of motion may increase, which can affect stability. AOs can create sagittal and frontal stability, leading to improved postural control [38]. Fu et al. suggested that incorrect positioning of the ankle while standing can lead to frequent sprains [48]. Researchers attribute this decline in postural control to impaired proprioception and the destruction of mechanoreceptors responsible for kinesthetic awareness of ankle positioning [49]. Some authors believe that orthoses improve postural control by increasing proprioception of the ankle joint. Additionally, AOs enhance tactile sensation on the plantar surface of the foot and reduce muscle strain at the ankle joint. Therefore, AOs can improve postural control by applying sensorimotor effects [40, 42].
Dynamic postural control
There is conflicting information about the impact of AOs on dynamic postural control in LAS. Some studies have found a positive effect of AOs on dynamic postural control [32, 36-39, 42, 43], while others have found them to be ineffective or even negative [32, 34, 41]. The variation in measurement techniques employed in various studies (including methods, such as force plates [30-35, 39, 40, 42], Biodex [36, 43], and clinical tests [37, 40-43], the diverse types of AOs (including soft [35-37, 41-44], semirigid [32, 37, 38], and rigid [30], and the heterogeneous study populations (encompassing individuals with acute injuries [30, 34, 38, 44], functional LAS [31, 32, 35, 37], or chronic ankle sprain [34, 36, 39, 40-44] could account for the lack of consistent findings across different studies. Some authors argue that the restriction in ankle range of motion caused by these orthoses may be the reason for their ineffectiveness or negative impact on dynamic postural control [34].
Comparison of orthoses
The findings from studies comparing the effectiveness of AOs have been inconsistent. Two studies found that a soft orthosis was more effective than a semi-rigid one in improving dynamic postural control [35, 42], while other studies reported that it had similar effects to the semi-rigid orthosis [32], or no effect at all [41]. One possible explanation for these discrepancies could be the inconsistent categorization of ankle sprain severity across studies. Additionally, comparisons between soft, semi-rigid, and customized AOs have demonstrated that customized orthoses yield greater postural control improvements [40].
Suggestions for future studies
1-Research on the impact of orthoses on various patient populations indicates that custom orthoses tailored to an individual’s biomechanics are more effective in enhancing patients’ health-related parameters compared to off-the-shelf orthoses. However, when it comes to individuals with ankle sprains, only two studies have explored the effects of custom orthoses. This suggests a need for further investigation into the design, production, and evaluation of custom orthoses for this specific patient group.
2-Given the conflicting findings in the existing literature, we recommend conducting additional research to thoroughly assess the effectiveness of AOs in enhancing dynamic postural control.
3-Many studies have primarily focused on the immediate effects of AOs, making it challenging to ascertain their long-term impact. Therefore, it is crucial to investigate and understand the prolonged effects of AOs.
4-Individuals with CAI often encounter both mechanical and functional limitations. Consequently, there is a necessity to develop and assess AOs that target the sensory system, aiming to enhance motor function in this particular population.
Conclusion
In summary, it appears that AOs, regardless of their type, demonstrate effectiveness in improving static postural control. However, the findings concerning their influence on dynamic postural control remain inconsistent. Comparative studies comparing soft and semi-rigid orthoses have generated contradictory results, leaving uncertainty about which type is more effective in enhancing postural control.
Limitations
As this study involved a review, it presented available data on the use of AOs to enhance postural control in patients with acute, chronic, and functional LAS. Further research in this area is essential to identify the most suitable AO, standardize tests, and evaluate postural control for improved comparisons. Varying significance levels (P<0.01 or P<0.05) among the studies made it challenging to statistically compare conflicting results across different studies. In different studies, varied parameters obtained from COP movements were used to evaluate postural control, making it impossible for us to compare articles based on outcome measure variables.
Ethical Considerations
Compliance with ethical guidelines
This systematic review study is regarded exclusively on published literature.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors
Authors' contributions
All authors adequately contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
References
Background of the population
Epidemiological research has indicated that lateral ankle sprains (LAS) are among the most frequent lower limb injuries in physically active individuals [1]. A sprain occurs when a ligament undergoes significant force or strain. The most common mechanism of this injury is a combination of plantarflexion and inversion movements with high velocity and torque [2]. Patients who have experienced an acute LAS are five times more likely to experience a repeat sprain [3], and over 40% of these individuals subsequently suffer from chronic ankle instability (CAI) [4, 5]. Researchers believe that CAI-related disorders originate from the primary damage that occurs during the initial sprain [6]. Patients with a history of significant LAS, recurrent sprains, episodes of ankle giving way, sensations of instability, or a decline in ankle function that persists for over a year may exhibit evidence of this condition [7, 8]. Long-term consequences, like ankle joint osteoarthritis, have been reported for individuals suffering from this condition [9]. Hiller et al. proposed a model for CAI, in which affected individuals are classified into three subgroups: Functional ankle instability (FAI), mechanical ankle instability (MAI), and repeated sprains [10]. MAI results in an expansion of the joint range of motion beyond the normal physiological level. It manifests as excessive inversion laxity of the rearfoot or excessive anterior laxity of the talocrural joint [11]. Functional instability in individuals with sprained ankles is due to disturbances in proprioceptive sense [12], skin sense [13-15], speed of nerve conduction [16], and neuromuscular response [12]. Damage to mechanoreceptors and nerve endings in the capsule, ligament, and ankle joint causes such instability [17].
Therefore, after the initial injury, different changes and defects occur at different levels of the neuromuscular system of the ankle and foot complex, and the multi-jointed nature of the complex as the base of the kinetic chain of the body causes more complications. Changes in CAI lead to extensive disorders, such as altered osteokinematics and muscle activity [18], which result in a change in postural control [12].
Ankle orthoses (AOs) and their effects
Due to the high prevalence of LAS and the large number of people who report subsequent CAI, it is necessary to manage the injury with rehabilitation interventions to compensate for or correct the disorders related to this complication. The usual treatment methods used are physiotherapy exercises [19], taping [20], and orthoses [21]. Most people prefer to use orthoses because doing physiotherapy exercises is time-consuming, and the tapes lose their effect after 10-40 minutes [22].
One of the most common clinical management approaches to acute and chronic ankle sprains is using AOs. It has been shown that these orthoses prevent primary and repeated injuries to the lateral ligaments and are usually used in CAI to increase the stability of the ankle joint. Using AOs leads to a 70% reduction in acute sprains among people with previous injuries and a 57% reduction among high school athletes without ankle injuries [23, 24]. Although the exact mechanism of injury prevention during orthosis use is unknown, the most prominent explanation involves sensory and mechanical effects. The mechanical effects are restriction of ankle and foot complex movements, while the sensory effects are caused by skin and mechanoreceptor stimulation, leading to proprioception improvement [25, 26].
Rationale
There have been several systematic reviews on the effectiveness of therapeutic interventions for LAS, indicating a high interest among researchers in finding the optimal treatment for this complication [27]. The effects of AOs on ankle biomechanics during changing directions, running, and landing have been investigated in two systematic studies [28, 29]. The first study looked at the effects of AOs on ankle biomechanics during a change of direction [28], while the second investigated the effects of AOs on peroneus longus muscle activity during sudden inversion in people with an ankle sprain [29]. However, the impact of AOs on postural control in individuals with acute, chronic, and functional LAS remains unclear. This systematic review aimed to determine whether AOs improve postural control in subjects with LAS.
Materials and Methods
Search method
To conduct the search, relevant keywords were chosen, and their synonyms were identified through the MeSH database. Then, following the population, intervention, comparison, outcome measure (PICO) protocol and using Boolean logical operators, a search term was created (Figure 1). In May 2023, a systematic search was carried out using the search term on PubMed, Web of Science, and Scopus databases. The search scope was limited to titles, keywords, and abstracts across all databases.
Eligibility criteria and selection process
This systematic study was done based on the PRISMA flow diagram. After the initial search, the title, keywords, and abstract of all the articles in English indexed in the reputable journals listed in the three databases were entered into the Endnote software, version 20.5.0. All these articles were published after peer review. The selection of articles was done by following the process mentioned below:
1) All duplicate articles were removed.
2) The title, keywords, and abstract were reviewed by three researchers based on the following criteria:
Inclusion criteria:
• Patients were individuals with acute, functional, or chronic LAS.
• The intervention used included various types of AOs.
• The outcome measures included all the variables that can be attributed to postural control based on the available documentation.
• Comparing the effects of the intervention on a group of individuals with CAI, FAI, and acute LAS with a control group, or with the contralateral healthy leg or with pre-intervention conditions.
Exclusion criteria:
• The studied population had sprains caused by musculoskeletal disorders or comorbidities such as ligament laxity.
• Patients received other conservative interventions such as physical therapy or non-steroidal anti-inflammatory drugs.
• Articles published as letters to the editor and commentary.
• Articles that studied animals.
3) The full texts of the included articles were obtained. Then, by reviewing the references of the articles, other articles deemed suitable were also retrieved.
4) The full texts of these articles were screened again by three reviewers according to the predefined inclusion criteria.
In cases where there was a disagreement between three authors on enlisting an article, other authors made the final decision.
Assessing the quality of articles
The studies included in this systematic review were rated as level 2 or higher according to the National Health and Medical Research Council (NHMRC). The selected papers were assessed using the physiotherapy evidence database (PEDro) scale, which consists of 11 criteria. Each criterion is answered with a yes or no, with a score of one assigned for yes answers and zero for no answers. The final score was calculated between 1 and 10 without considering the first item. Methodological quality was determined as follows: Studies scoring 0-4 were considered poor, 4-5 were fair, 6-8 were good, and studies scoring 9-10 were excellent.
Data extraction, presentation, and analysis
Information was extracted from each included trial on: 1) Characteristics of the trial (mean age, gender, history of acute LAS/FAI/CAI) and control group (healthy group, randomized allocation, or without control group) participants; 2) Type and characteristics of AOs; 3) Type of outcome measures (COP parameters, clinical tests, and indices related to dynamic postural control). Also, the information related to study design, assessment protocol, and final conclusions were collected from the studies. There was no data pooling or meta-analysis because the included studies did not all use the -same protocols, assessment tools, foot condition (barefoot or wearing shoes), or definition of LAS (acute, functional, or chronic).
Results
Study selection
After conducting the initial search, we found 156 articles. However, after following the steps outlined in the PRISMA flowchart, only 14 articles met the necessary criteria for this study (Figure 2).
Methodological quality assessment
After examining the level of studies according to the NHMRC classification, two studies were at level 2 (having at least one properly designed RCT) [38, 42], and the rest were at level 3 (controlled trial without randomization).
In this study, the quality of the methodology was evaluated using PEDro’s scale (Table 1).
Results showed that all studies had identified eligibility criteria, obtained results from more than 85% of participants, and reported diversity criteria. However, the risk of bias in the studies was very high regarding randomization and blinding. Furthermore, only one of the studies, which was an RCT, explained the attrition rate and its cause. Figure 3 displays the overall results of PEDro’s checklist items as percentages.
Study characteristics
The text below presents the search results from the articles included in this study, categorized based on the characteristics of the samples, interventions, and outcomes. The study’s features are outlined in Table 2.
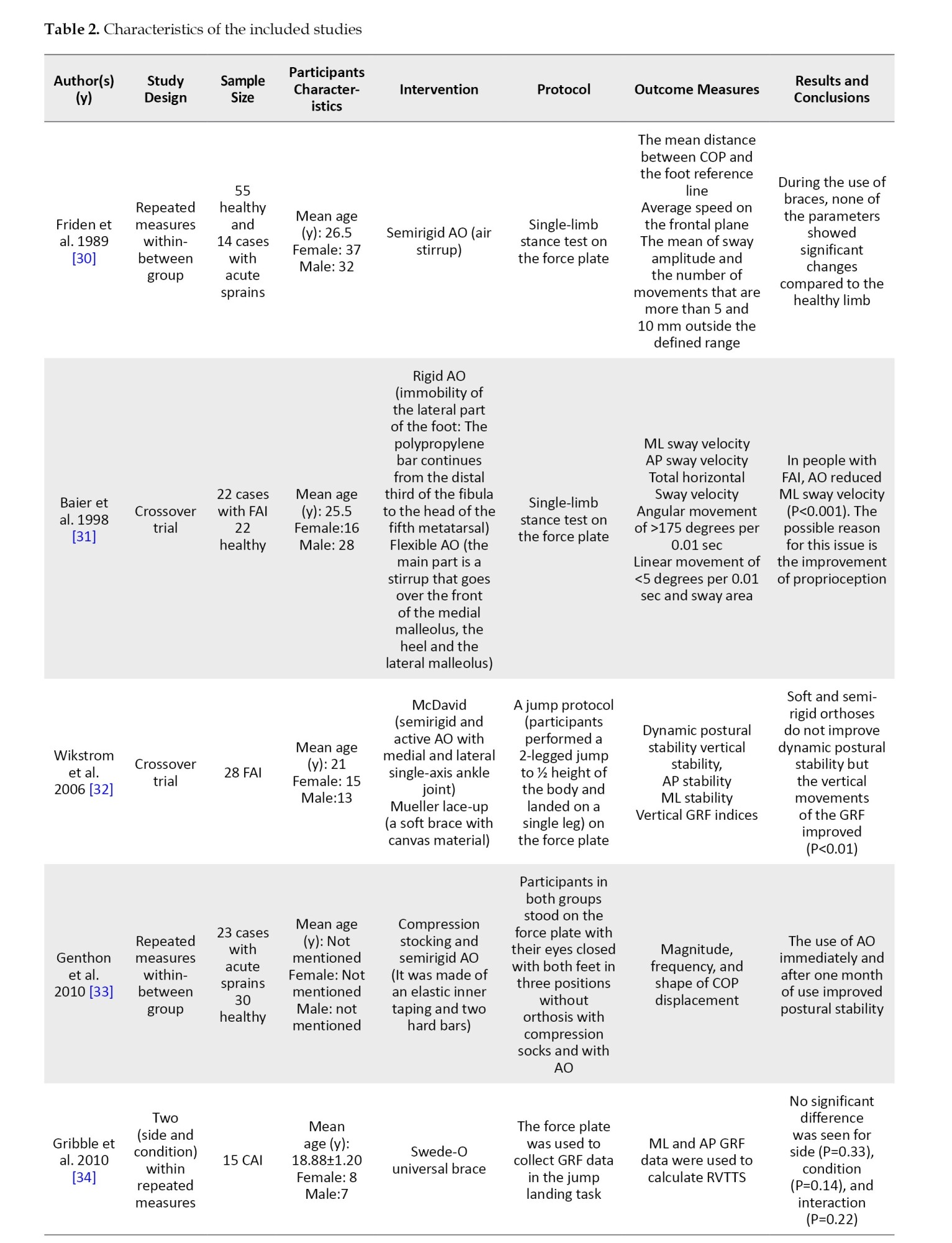


Participant’s characteristics
The studies involved a total of 678 participants, of whom 96 had acute sprains, 86 had FAI, and 172 had CAI. Additionally, 324 healthy individuals were included as part of the control group. The size of each sample varied from 15 to 124, with a mean of 45 people per study. The overall mean age of the participants was 23.4 years, except for one study where the mean age of the samples was not reported.
Interventions
Different terms were used to describe the types of AOs. Generally, AOs used in studies were divided into two types: Customized and prefabricated. In 12 studies, prefabricated AOs were used, while in two studies, customized types were used. Customized AOs were made according to the size of the individual’s foot and ankle complex, which was composed of a combination of a soft ankle sleeve, footplate, and ML stirrup support [39, 40].
The most common method of categorizing prefabricated AOs was based on the hardness of the materials used. Accordingly, AOs were divided into three categories: Rigid, semi-rigid, and soft. The rigid type had a hard lateral section of polyethylene that originated from the distal third of the fibula and terminated at the head of the 5th metatarsal. This orthosis aims to significantly reduce inversion, eversion, plantarflexion, and dorsiflexion movements [30, 38]. The semi-rigid type is typically made of a layer of neoprene [36, 40], canvas [37, 39], nylon [35, 44], and two-sided bars or U-shaped stirrups [37-39]. Additionally, in the active AO, which is considered a semi-rigid type, there are single-axis joints at each side of the ankle [36, 40-42], resulting from the connection of U-shaped stirrups with the lateral bars. Semi-rigid AOs allow movement in the sagittal plane while preventing inversion and eversion [37]. The soft type is usually made of a layer of neoprene [36], nylon [37, 39, 42], or canvas [30-32] and may have a double-sided spring [35, 37, 39] for relative lateral and medial support. The purpose of making soft AOs is to provide support and slightly reduce the movements of the ankle joint at the end of the ankle’s range of motion in different planes [44]. To secure these orthoses on the ankle, various fastening methods (circumferential [43], figure-of-eight [32, 39, 40], triple-stitched straps [42], and lace-up [30, 31] were used.
Outcomes
In this section, we categorized the different variables that the researchers measured and associated with the concept of postural control.
COP parameters
In three studies [35, 39, 40], the Mean±SD total velocity in anteroposterior (AP) direction, SD of velocity in mediolateral (ML) direction, phase plane portrait, phase plane portrait AP, and phase plane portrait ML were used as parameters for measuring static postural control. The impact of soft, semirigid, and combined mechanism ankle support (CMAS) orthoses on these parameters was assessed, and it was found that there were significant improvements in the phase plane portrait (F(2, 38)=4.32, P=0.03), mean total velocity (F(2, 38)=4.60, P=0.02) [35], and all COP parameters (P˂0.02) [39], respectively. Furthermore, the results of a post hoc test indicated that CMAS had a significant decrease in all COP parameters (P˂0.05) compared to soft AO and foot orthoses (FO) [40].
In two studies [30, 31], different COP parameters were used to check postural control. These included sway area, ML sway velocity, AP sway velocity, total horizontal sway velocity, angular movement of >175 degrees per 0.01 sec, and lineal movement of <5 degrees per 0.01 sec. Soft (P˂0.001) and semi-rigid (P=0.002) AOs in the FAI group significantly affected ML sway velocity. The soft orthosis significantly reduced lineal movement by <5 degrees per 0.01 sec (P=0.002) [31].
Genthon et al. [33] considered magnitude, frequency, and displacement shape as COP parameters. They found that the shape of displacement (P˂0.05) and magnitude (P˂0.001) in the semirigid AO group were significantly lower than those in the compression stockings and no orthosis groups.
Best et al. [38] used the sum of frontal and sagittal COP movements in each time unit to obtain the total oscillation distance. This method found no difference between rigid and semirigid orthoses in improving postural control.
Clinical tests
In five studies [37, 40-43] the star excursion balance test (SEBT) was used to evaluate dynamic postural control. The comparison of soft and semirigid orthoses showed a significant increase in distance difference in the posteromedial (5% difference, P˂0.05) [37], anterior (0.048), and anterolateral (P=0.046) directions when using the soft one [43]. When comparing CMAS with soft AO and FO, it was observed that the reaching distance increased in the medial direction (P=0.022 in the comparison between FO and CMAS) and anteromedial direction (P=0.046 in the comparison between FO and CMAS, and P=0.042 in the comparison between soft AO and CMAS) when CMAS was utilized [40]. However, a study by John et al. [41] found that soft AO had no impact on the Y balance test [41].
In a study [42], the single leg stance test (SLST) was used to evaluate static postural control. The results revealed no significant differences in the use of soft, semi-rigid AOs, or Kinesio tape. Additionally, the same study utilized the Single Hop Test and Y balance test to evaluate dynamic postural control, and the findings indicated that the measured distance did not significantly differ when using soft, semi-rigid AOs, or Kinesio tape.
Indexes related to dynamic postural control
Some of the indices used to compare control, soft AOs, and semi-rigid AOs were vertical stability, AP stability, ML stability, and dynamic postural stability. The results showed that the use of soft and semi-rigid AOs led to a significant improvement in the vertical GRF index (P<0.01) [32]. When using the Biodex device, it was found that both soft and semi-rigid AOs significantly improved the dynamic (F=5.1, P=0.01) and semi-dynamic (F=6.2, P<0.001) indices compared to the group without orthosis [36].
Hassanpour et al. compared soft and semi-rigid AOs by calculating AP stability, ML stability, and overall stability indices and found no difference between the two groups [43]. In another study, Gribble et al. calculated the resultant vector time to stabilization (RVTTS) index using AP and ML GRF data. The researchers discovered that using an AO did not significantly affect this index [34]. Additionally, the use of elastic AOs in individuals with CAI did not result in improved performance on the landing error scoring system (LESS) or balance error scoring system (BESS) [41].
Discussion
The recovery of postural control is the foundation of rehabilitation following LAS [44]. AOs are frequently utilized in sports to enhance postural control, and they are widely accepted and utilized due to their ease of use, adjustability, and reasonable price [45]. AOs are complex biomechanical interventions that vary in terms of materials, fastening methods, and their ability to create stability [46].
Static postural control
Some studies found AOs to be effective in improving static postural control in subjects with LAS [30, 31, 35, 39, 40, 42], but John et al. said that elastic AO was not effective in improving static or dynamic postural control [41]. One possible explanation for the conflicting results may be the reliability of the BESS used in Johns et al.’s study [41]. Finnoff et al. reported that the inter-rater reliability of BESS is poor [47]. Additionally, Best et al. believe that semirigid AOs are not effective in improving postural control after LAS. They investigated the effect of this orthosis on postural control in individuals with acute sprains and obtained conflicting results compared to those with chronic or functional sprains [38].
Based on research findings, AOs are effective in improving static postural control. After an ankle sprain, the range of motion may increase, which can affect stability. AOs can create sagittal and frontal stability, leading to improved postural control [38]. Fu et al. suggested that incorrect positioning of the ankle while standing can lead to frequent sprains [48]. Researchers attribute this decline in postural control to impaired proprioception and the destruction of mechanoreceptors responsible for kinesthetic awareness of ankle positioning [49]. Some authors believe that orthoses improve postural control by increasing proprioception of the ankle joint. Additionally, AOs enhance tactile sensation on the plantar surface of the foot and reduce muscle strain at the ankle joint. Therefore, AOs can improve postural control by applying sensorimotor effects [40, 42].
Dynamic postural control
There is conflicting information about the impact of AOs on dynamic postural control in LAS. Some studies have found a positive effect of AOs on dynamic postural control [32, 36-39, 42, 43], while others have found them to be ineffective or even negative [32, 34, 41]. The variation in measurement techniques employed in various studies (including methods, such as force plates [30-35, 39, 40, 42], Biodex [36, 43], and clinical tests [37, 40-43], the diverse types of AOs (including soft [35-37, 41-44], semirigid [32, 37, 38], and rigid [30], and the heterogeneous study populations (encompassing individuals with acute injuries [30, 34, 38, 44], functional LAS [31, 32, 35, 37], or chronic ankle sprain [34, 36, 39, 40-44] could account for the lack of consistent findings across different studies. Some authors argue that the restriction in ankle range of motion caused by these orthoses may be the reason for their ineffectiveness or negative impact on dynamic postural control [34].
Comparison of orthoses
The findings from studies comparing the effectiveness of AOs have been inconsistent. Two studies found that a soft orthosis was more effective than a semi-rigid one in improving dynamic postural control [35, 42], while other studies reported that it had similar effects to the semi-rigid orthosis [32], or no effect at all [41]. One possible explanation for these discrepancies could be the inconsistent categorization of ankle sprain severity across studies. Additionally, comparisons between soft, semi-rigid, and customized AOs have demonstrated that customized orthoses yield greater postural control improvements [40].
Suggestions for future studies
1-Research on the impact of orthoses on various patient populations indicates that custom orthoses tailored to an individual’s biomechanics are more effective in enhancing patients’ health-related parameters compared to off-the-shelf orthoses. However, when it comes to individuals with ankle sprains, only two studies have explored the effects of custom orthoses. This suggests a need for further investigation into the design, production, and evaluation of custom orthoses for this specific patient group.
2-Given the conflicting findings in the existing literature, we recommend conducting additional research to thoroughly assess the effectiveness of AOs in enhancing dynamic postural control.
3-Many studies have primarily focused on the immediate effects of AOs, making it challenging to ascertain their long-term impact. Therefore, it is crucial to investigate and understand the prolonged effects of AOs.
4-Individuals with CAI often encounter both mechanical and functional limitations. Consequently, there is a necessity to develop and assess AOs that target the sensory system, aiming to enhance motor function in this particular population.
Conclusion
In summary, it appears that AOs, regardless of their type, demonstrate effectiveness in improving static postural control. However, the findings concerning their influence on dynamic postural control remain inconsistent. Comparative studies comparing soft and semi-rigid orthoses have generated contradictory results, leaving uncertainty about which type is more effective in enhancing postural control.
Limitations
As this study involved a review, it presented available data on the use of AOs to enhance postural control in patients with acute, chronic, and functional LAS. Further research in this area is essential to identify the most suitable AO, standardize tests, and evaluate postural control for improved comparisons. Varying significance levels (P<0.01 or P<0.05) among the studies made it challenging to statistically compare conflicting results across different studies. In different studies, varied parameters obtained from COP movements were used to evaluate postural control, making it impossible for us to compare articles based on outcome measure variables.
Ethical Considerations
Compliance with ethical guidelines
This systematic review study is regarded exclusively on published literature.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors
Authors' contributions
All authors adequately contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
References
- Herzog MM, Kerr ZY, Marshall SW, Wikstrom EA. Epidemiology of ankle sprains and chronic ankle instability. Journal of Athletic Training. 2019; 54(6):603-10. [DOI:10.4085/1062-6050-447-17] [PMID] [PMCID]
- Kobayashi T, Tanaka M, Shida M. Intrinsic risk factors of lateral ankle sprain: A systematic review and meta-analysis. Sports Health. 2016; 8(2):190-3. [DOI:10.1177/1941738115623775] [PMID] [PMCID]
- McKay GD, Goldie PA, Payne WR, Oakes BW. Ankle injuries in basketball: Injury rate and risk factors. British Journal of Sports Medicine. 2001; 35(2):103-8. [DOI:10.1136/bjsm.35.2.103] [PMID] [PMCID]
- Doherty C, Bleakley C, Hertel J, Caulfield B, Ryan J, Delahunt E. Recovery from a first-time lateral ankle sprain and the predictors of chronic ankle instability: A prospective cohort analysis. The American Journal of Sports Medicined. 2016; 44(4):995-1003. [DOI:10.1177/0363546516628870] [PMID]
- Doherty C, Delahunt E, Caulfield B, Hertel J, Ryan J, Bleakley C. The incidence and prevalence of ankle sprain injury: A systematic review and meta-analysis of prospective epidemiological studies. Sports Medicine. 2014; 44(1):123-40. [DOI:10.1007/s40279-013-0102-5] [PMID]
- Miklovic TM, Donovan L, Protzuk OA, Kang MS, Feger MA. Acute lateral ankle sprain to chronic ankle instability: A pathway of dysfunction. The Physician and Sportsmedicine. 2018; 46(1):116-22. [DOI:10.1080/00913847.2018.1409604] [PMID]
- Hertel J. Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. Journal of Athletic Training. 2002; 37(4):364-75. [PMID] [PMCID]
- Gribble PA, Delahunt E, Bleakley C, Caulfield B, Docherty CL, Fourchet F, et al. Selection criteria for patients with chronic ankle instability in controlled research: A position statement of the international ankle consortium. The Journal of Orthopaedic and Sports Physical Therapy. 2013; 43(8):585-91. [DOI:10.2519/jospt.2013.0303] [PMID]
- van Ochten JM, de Vries AD, van Putte N, Oei EHG, Bindels PJE, Bierma-Zeinstra SMA, et al. Association between patient history and physical examination and osteoarthritis after ankle Sprain. International Journal of Sports Medicine. 2017; 38(9):717-24. [DOI:10.1055/s-0043-109554] [PMID]
- Hiller CE, Kilbreath SL, Refshauge KM. Chronic ankle instability: Evolution of the model. Journal of Athletic Training. 2011; 46(2):133-41. [DOI:10.4085/1062-6050-46.2.133] [PMID] [PMCID]
- Delahunt E, Coughlan GF, Caulfield B, Nightingale EJ, Lin CW, Hiller CE. Inclusion criteria when investigating insufficiencies in chronic ankle instability. Medicine and Science in Sports and Exercise. 2010; 42(11):2106-21. [DOI:10.1249/MSS.0b013e3181de7a8a] [PMID]
- Munn J, Sullivan SJ, Schneiders AG. Evidence of sensorimotor deficits in functional ankle instability: A systematic review with meta-analysis. Journal of Science and Medicine in Sport. 2010; 13(1):2-12. [DOI:10.1016/j.jsams.2009.03.004] [PMID]
- Burcal CJ, Wikstrom EA. Plantar cutaneous sensitivity with and without cognitive loading in people with chronic ankle instability, copers, and uninjured controls. The Journal of Orthopaedic and Sports Physical Therapy. 2016; 46(4):270-6. [DOI:10.2519/jospt.2016.6351] [PMID]
- Hoch MC, McKeon PO, Andreatta RD. Plantar vibrotactile detection deficits in adults with chronic ankle instability. Medicine and Science in Sports and Exercise. 2012; 44(4):666-72. [DOI:10.1249/MSS.0b013e3182390212] [PMID]
- Powell MR, Powden CJ, Houston MN, Hoch MC. Plantar cutaneous sensitivity and balance in individuals with and without chronic ankle instability. Clinical Journal of Sport Medicine. 2014; 24(6):490-6. [DOI:10.1097/JSM.0000000000000074] [PMID]
- Simon J, Docherty C. Slower nerve conduction velocity in individuals with functional ankle instability. International Journal of Sports Medicine. 2014; 35(9):731-6. [DOI:10.1055/s-0033-1361183] [PMID]
- Freeman MAR, Dean MR, Hanham IW. The etiology and prevention of functional instability of the foot. The Bone & Joint Journal. 1965; 47(4):678-85. [DOI:10.1302/0301-620X.47B4.678]
- Moisan G, Descarreaux M, Cantin V. Effects of chronic ankle instability on kinetics, kinematics and muscle activity during walking and running: A systematic review. Gait & Posture. 2017; 52:381-99. [DOI:10.1016/j.gaitpost.2016.11.037] [PMID]
- van der Wees PJ, Lenssen AF, Hendriks EJ, Stomp DJ, Dekker J, de Bie RA. Effectiveness of exercise therapy and manual mobilisation in ankle sprain and functional instability: A systematic review. The Australian Journal of Physiotherapy. 2006; 52(1):27-37. [DOI:10.1016/S0004-9514(06)70059-9] [PMID]
- Raymond J, Nicholson LL, Hiller CE, Refshauge KM. The effect of ankle taping or bracing on proprioception in functional ankle instability: A systematic review and meta-analysis. Journal of Science and Medicine in Sport. 2012; 15(5):386-92. [DOI:10.1016/j.jsams.2012.03.008] [PMID]
- Dizon JM, Reyes JJ. A systematic review on the effectiveness of external ankle supports in the prevention of inversion ankle sprains among elite and recreational players. Journal of Science and Medicine in Sport. 2010; 13(3):309-17. [DOI:10.1016/j.jsams.2009.05.002] [PMID]
- Richie DH Jr. Functional instability of the ankle and the role of neuromuscular control: A comprehensive review. The Journal of Foot and Ankle Surgery. 2001; 40(4):240-51. [DOI:10.1016/S1067-2516(01)80025-9] [PMID]
- McGuine TA, Brooks A, Hetzel S. The effect of lace-up ankle braces on injury rates in high school basketball players. The American Journal of Sports Medicine. 2011; 39(9):1840-8. [DOI:10.1177/0363546511406242] [PMID] [PMCID]
- McGuine TA, Hetzel S, Wilson J, Brooks A. The effect of lace-up ankle braces on injury rates in high school football players. The American Journal of Sports Medicine. 2012; 40(1):49-57. [DOI:10.1177/0363546511422332] [PMID] [PMCID]
- Papadopoulos E, Nicolopoulos C, Anderson E, Curran M, Athanasopoulos S. The role of ankle bracing in injury prevention, athletic performance and neuromuscular control: A review of the literature. The Foot. 2005; 15(1):1-6. [DOI:10.1016/j.foot.2004.07.002]
- Cordova ML, Ingersoll CD, Palmieri RM. Efficacy of prophylactic ankle support: An experimental perspective. Journal of Athletic Training. 2002; 37:446-57. [PMID] [PMCID]
- Doherty C, Bleakley C, Delahunt E, Holden S. Treatment and prevention of acute and recurrent ankle sprain: An overview of systematic reviews with meta-analysis. British Journal of Sports Medicine. 2017; 51(2):113-25. [DOI:10.1136/bjsports-2016-096178] [PMID]
- Rowe PL, Bryant AL, Egerton T, Paterson KL. External ankle support effects on ankle biomechanics in chronic ankle instability: Systematic review and meta-analysis. Medicine & Science in Sports & Exercise. 54(9S):440. [DOI:10.1249/01.mss.0000880584.18731.88]
- Plangtaisong P, Shen W, Wheeler PC, Fong DT. Effect of exercise interventions and prophylactic devices on reducing peroneal muscle reaction time by sudden ankle perturbation: A systematic review and meta-analysis. Medicine in Novel Technology and Devices. 2021; 11:100082. [DOI:10.1016/j.medntd.2021.100082]
- Fridén T, Zätterström R, Lindstrand A, Moritz U. A stabilometric technique for evaluation of lower limb instabilities. The American Journal of Sports Medicine. 1989; 17(1):118-22. [DOI:10.1177/036354658901700120] [PMID]
- Baier M, Hopf T. Ankle orthoses effect on single-limb standing balance in athletes with functional ankle instability. Archives of Physical Medicine and Rehabilitation. 1998; 79(8):939-44. [DOI:10.1016/S0003-9993(98)90091-0] [PMID]
- Wikstrom EA, Arrigenna MA, Tillman MD, Borsa PA. Dynamic postural stability in subjects with braced, functionally unstable ankles. Journal of Athletic Training. 2006; 41(3):245. [PMID] [PMCID]
- Genthon N, Bouvat E, Banihachemi JJ, Bergeau J, Abdellaoui A, Rougier PR. Lateral ankle sprain alters postural control in bipedal stance: Part 2 sensorial and mechanical effects induced by wearing an ankle orthosis. Scandinavian Journal of Medicine & Science in Sports. 2010; 20(2):255-61. [DOI:10.1111/j.1600-0838.2009.00932.x] [PMID]
- Gribble PA, Taylor BL, Shinohara J. Bracing does not improve dynamic stability in chronic ankle instability subjects. Physical Therapy in Sport. 2010; 11(1):3-7. [DOI:10.1016/j.ptsp.2009.11.003] [PMID]
- Hadadi M, Mazaheri M, Mousavi ME, Maroufi N, Bahramizadeh M, Fardipour S. Effects of soft and semi-rigid ankle orthoses on postural sway in people with and without functional ankle instability.Journal of Science and Medicine in Sport. 2011; 14(5):370-5. [DOI:10.1016/j.jsams.2010.12.004] [PMID]
- Faraji E, Daneshmandi H, Atri AE, Onvani V, Namjoo FR. Effects of prefabricated ankle orthoses on postural stability in basketball players with chronic ankle instability. Asian Journal of Sports Medicine. 2012; 3(4):274-8. [DOI:10.5812/asjsm.34551] [PMID] [PMCID]
- Hadadi M, Mousavi ME, Fardipour S, Vameghi R, Mazaheri M. Effect of soft and semirigid ankle orthoses on Star Excursion Balance Test performance in patients with functional ankle instability. Journal of Science and Medicine in Sport. 2014; 17(4):430-3. [DOI:10.1016/j.jsams.2013.05.017] [PMID]
- Best R, Böhle C, Schiffer T, Petersen W, Ellermann A, Brueggemann GP, Liebau C. Early functional outcome of two different orthotic concepts in ankle sprains: A randomized controlled trial. Archives of Orthopaedic and Trauma Surgery. 2015; 135(7):993-1001. [DOI:10.1007/s00402-015-2230-x] [PMID]
- Hadadi M, Ebrahimi I, Mousavi ME, Aminian G, Esteki A, Rahgozar M. The effect of combined mechanism ankle support on postural control of patients with chronic ankle instability. Prosthetics and Orthotics International. 2017; 41(1):58-64. [DOI:10.1177/0309364615596068] [PMID]
- Hadadi M, Abbasi F. Comparison of the effect of the combined mechanism ankle support on static and dynamic postural control of chronic ankle instability patients. Foot & Ankle International. 2019; 40(6):702-9. [DOI:10.1177/1071100719833993] [PMID]
- John C, Stotz A, Gmachowski J, Rahlf AL, Hamacher D, Hollander K, et al. Is an elastic ankle support effective in improving jump landing performance, and static and dynamic balance in young adults with and without chronic ankle instability? Journal of Sport Rehabilitation. 2019; 29(6):789-94. [DOI:10.1123/jsr.2019-0147] [PMID]
- Hadadi M, Haghighat F, Mohammadpour N, Sobhani S. Effects of kinesiotape vs soft and semirigid ankle orthoses on balance in patients with chronic ankle instability: A randomized controlled trial. Foot & Ankle International. 2020; 41(7):793-802. [DOI:10.1177/1071100720917181] [PMID]
- Hassanpour S, Daryabor A, Jamshidi A, Rezaei M. Efficacy of ankle supports on dynamic postural control in patients with chronic ankle instability. Journal of Prosthetics and Orthotics. 2020; 32(3):194-202. [DOI:10.1097/JPO.0000000000000309]
- Massion J. Postural control system. Current Opinion in Neurobiology. 1994; 4(6):877-87. [DOI:10.1016/0959-4388(94)90137-6] [PMID]
- Khaliliyan H, Sharafatvaziri A, Safaeepour Z, Bahramizadeh M. Gait and muscle activity measures after biomechanical device therapy in subjects with ankle instability: A systematic review. The Foot. 2024; 102083. [DOI: 10.1016/j.foot.2024.102083] [PMID]
- Feuerbach JW, Grabiner MD, Koh TJ, Weiker GG. Effect of an ankle orthosis and ankle ligament anesthesia on ankle joint proprioception. The American Journal of Sports Medicine. 1994; 22(2):223-9. [DOI:10.1177/036354659402200212] [PMID]
- Finnoff JT, Peterson VJ, Hollman JH, Smith J. Intrarater and interrater reliability of the balance error scoring system (BESS). PM & R. 2009; 1(1):50-4. [DOI:10.1016/j.pmrj.2008.06.002] [PMID]
- Fu AS, Hui-Chan CW. Ankle joint proprioception and postural control in basketball players with bilateral ankle sprains. The American Journal of Sports Medicine. 2005; 33(8):1174-82. [DOI:10.1177/0363546504271976] [PMID]
- Akbari M, Karimi H, Farahini H, Faghihzadeh S. Balance problems after unilateral lateral ankle sprains. Journal of Rehabilitation Research and Development. 2006; 43(7):819-24. [DOI:10.1682/JRRD.2006.01.0001] [PMID]
Article type: Reviews |
Subject:
Orthosis and Prosthesis
Received: 2024/01/6 | Accepted: 2024/01/11 | Published: 2024/03/1
Received: 2024/01/6 | Accepted: 2024/01/11 | Published: 2024/03/1
Send email to the article author




