Volume 23, Issue 4 (December 2025)
Iranian Rehabilitation Journal 2025, 23(4): 463-472 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Laftah S A, Hammooz A. Nurse-led Telehealth Follow-up as a Mediator Between Caregiver Burden and Functional Recovery of Stroke Patients. Iranian Rehabilitation Journal 2025; 23 (4) :463-472
URL: http://irj.uswr.ac.ir/article-1-2588-en.html
URL: http://irj.uswr.ac.ir/article-1-2588-en.html
1- Department of Community Health Nursing, College of Nursing, University of Thi-Qar, Thi-Qar, Iraq.
2- Department of Community Health Nursing, College of Nursing, University of AL-Qadisiyah, AL-Qadisiyah, Iraq.
2- Department of Community Health Nursing, College of Nursing, University of AL-Qadisiyah, AL-Qadisiyah, Iraq.
Keywords: Caregiver burden, Functional recovery, Telehealth usability, Mediation, Informal caregivers, Rural health
Full-Text [PDF 576 kb]
(257 Downloads)
| Abstract (HTML) (1349 Views)
Full-Text: (69 Views)
Introduction
Stroke remains a leading cause of long-term disability globally, frequently leaving survivors with significant physical, cognitive, and emotional impairments that necessitate continuous care [1]. Functional recovery in stroke patients is a complex process influenced by various factors, including exceptional post-discharge care and the pivotal role of informal caregivers [2]. Informal caregivers, typically family members, are instrumental in assisting stroke survivors through rehabilitation; however, they often experience excessive psychological, physical, and emotional burdens, which can negatively impact patient recovery outcomes [3, 4].
Recent research has consistently demonstrated a significant relationship between caregiver burden and functional recovery in stroke patients. Higher levels of burden are often linked to poorer patient outcomes, primarily due to reduced quality of care and increased caregiver burnout [5, 6]. Consequently, strategies aimed at alleviating caregiver burden and enhancing support mechanisms are crucial for improving patient recovery. One promising approach gaining increasing attention is the implementation of nurse-led telehealth interventions, which have proven effective in providing timely support, education, and monitoring for both patients and their caregivers [7, 8].
Nurse-led telehealth follow-up, typically encompassing remote consultations, health education, and ongoing monitoring by trained nurses, offers a valuable strategy to bridge existing gaps in post-discharge care [9, 10]. This approach not only enhances continuity of care but also empowers caregivers by offering guidance and emotional support, thereby potentially reducing their burden and positively influencing the patient’s rehabilitation [11, 12]. Furthermore, evidence suggests that such interventions improve self-management behaviors, medication adherence, and facilitate early detection of complications, all of which are critical for optimal stroke recovery [13].
Despite the growing body of literature supporting telehealth and caregiver support independently, there remains a notable gap in understanding the mediating role of nurse-led telehealth in the intricate relationship between caregiver burden and functional recovery in stroke patients. Exploring this mediating role is paramount for developing integrated care models and optimizing outcomes for both patients and caregivers. Therefore, this study aimed to investigate whether nurse-led telehealth follow-up can mediate caregiver burden and functional recovery among stroke patients.
Materials and Methods
Study design and setting
This study employed a cross-sectional, descriptive-correlational design. The primary objective was to examine the association between caregiver burden and functional recovery in patients with stroke, with a specific focus on the mediating role of network nurse-led telehealth follow-up. The research was conducted across multiple community-based rehabilitation facilities and outpatient neurology clinics affiliated with Al-Nasiriya Teaching Hospital, located in Thi-Qar Governorate, Iraq. The data collection period spanned from February 1st to June 30th, 2025. These specific healthcare settings were selected due to their established role in providing post-discharge rehabilitation and ongoing follow-up care for stroke survivors within the governorate. Their integration with community health nursing services and access to diverse patient populations made them ideal for gathering comprehensive data on caregiver experiences and patient recovery trajectories.
Study sample
A stratified random sampling method was utilized to ensure a representative sample of different types of informal caregivers for stroke survivors. Stratification was performed based on geographic area (urban vs rural) and type of healthcare facility (community health center vs outpatient clinic) to accurately reflect the region’s broader demographic and healthcare delivery patterns. The sample size was calculated using the formula for a single-population proportion. Based on an assumed incidence (p) of 30%, a 95% confidence level (Z=1.96), and a margin of error (d) of 0.05, the initial sample size (n₀) was determined to be 323. Considering the total eligible population of approximately 1200 stroke patients and their caregivers under follow-up, the final corrected sample size remained 323, ensuring adequate statistical power for the analyses.
Participants were eligible if they were 18 years or older, served as informal caregivers to a stroke patient discharged at least one month prior, and had participated in at least one network nurse-led telehealth follow-up session. Caregivers also required to understand Arabic sufficiently to provide informed consent and complete the study. Caregivers of patients with degenerative neurological conditions (Parkinson’s disease) or those with documented psychiatric illnesses that could impair their caregiving or response accuracy were excluded.
Study instruments
Three standardized and validated instruments were employed to collect data on the study variables:
Zarit burden interview-short version (ZBI-12)
This 12-item instrument measures caregivers’ perceived burden. Each item is rated on a 5-point Likert scale, ranging from 0 (never) to 4 (nearly always). The total score ranges from 0 to 48, with higher scores indicating greater caregiver burden. The Arabic version of the ZBI-12 has demonstrated robust internal consistency (Cronbach’s α=0.88) and good test re-test reliability (interclass correlation coefficient [ICC]=0.85) in Middle Eastern populations [13, 14].
Telehealth usability questionnaire (TUQ)
This 21-item scale assesses caregivers’ perceptions of the usability and effectiveness of telehealth services provided by community nurses. It covers multiple domains, including usefulness, ease of use, and interaction quality, with each item rated on a 7-point Likert scale. The Arabic version of the TUQ exhibited excellent psychometric properties in pilot testing (α=0.91, ICC=0.89), making it suitable for the study’s cultural and contextual settings [15].
Barthel index (BI)
The BI was used to assess the functional recovery of stroke patients, as reported by their caregivers. This 10-item instrument evaluates performance in basic activities of daily living, such as feeding, bathing, grooming, and mobility. The total score ranges from 0 (complete dependence) to 100 (complete independence). The Arabic version of the BI used in this study had been previously validated within the Iraqi healthcare system, and established studies show strong reliability (Cronbach’s α=0.95, ICC=0.93), confirming its widespread acceptance in stroke rehabilitation research [16].
Validity and reliability
To ensure cultural and linguistic appropriateness for the Iraqi context, all three instruments underwent a rigorous forward–backward translation process conducted by bilingual healthcare professionals experienced in both nursing and rehabilitation. The translated versions were subsequently reviewed by a panel of five academic and clinical experts in community health nursing to assess conceptual equivalence, readability, and content validity. A pilot study involving 30 caregivers (not included in the final sample) was conducted to test the instruments’ feasibility, readability, and internal consistency. The pilot results confirmed the suitability of these tools for the target population.
Data collection
Data were collected through self-administered questionnaires for literate participants and researcher-administered interviews for those with limited literacy. Data were collected in a private setting to ensure participant confidentiality. Trained data collectors with nursing backgrounds conducted the interviews in Arabic. Data collection occurred over four months (February 1st to June 30th, 2025) during routine outpatient rehabilitation or telehealth review clinic visits. Written informed consent was obtained from each participant prior to data collection. Ethical approval was obtained from the Scientific Research Ethics Committee of the College of Nursing, University of Thi-Qar. Participants were assured of confidentiality, voluntary participation, and their right to withdraw at any time without consequences to their care.
Data analysis
Data were analyzed using IBM SPSS software, version 26. Descriptive records, along with Mean±SD, frequencies, and probabilities, were used to summarize caregivers’ demographic traits, clinical data of stroke patients, and the total scores obtained from the ZBI, TUQ, and BI. The normality of continuous variables was assessed using the Kolmogorov-Smirnov and Shapiro-Wilk tests, along with visual inspection of histograms and assessment of skewness and kurtosis values. To examine the relationships among the primary study variables, Pearson’s correlation coefficient (r) was employed to determine the strength and direction of the bivariate associations among caregiver burden, telehealth observation usability, and functional recovery of stroke patients. Mediation analysis was performed using Hayes’ PROCESS macro (model 4) to assess the mediating role of community nurse-led telehealth follow-up (TUQ) in the relationship between caregiver burden (ZBI) and functional recovery (BI). The indirect effect was tested using a bootstrapping approach with 5,000 resamples to generate bias-corrected 95% confidence intervals (CI). Mediation was statistically significant when the confidence interval did not include zero. A P<0.05 was the threshold for statistical significance in some analyses.
Results
Table 1 presents the demographic characteristics of the informal caregivers. The Mean±SD age of the caregivers was 41.3±10.2 years. Most caregivers were female (73.7%) and married (81.7%). Educational attainment varied, with 38.1% having completed secondary education and 33.7% holding a university degree or higher. A significant portion (72.8%) was unemployed, potentially reflecting the demands of caregiving. The most common relationship to the patient was spouse (34.7%) and child (29.7%). Geographically, most caregivers resided in urban areas (63.2%).
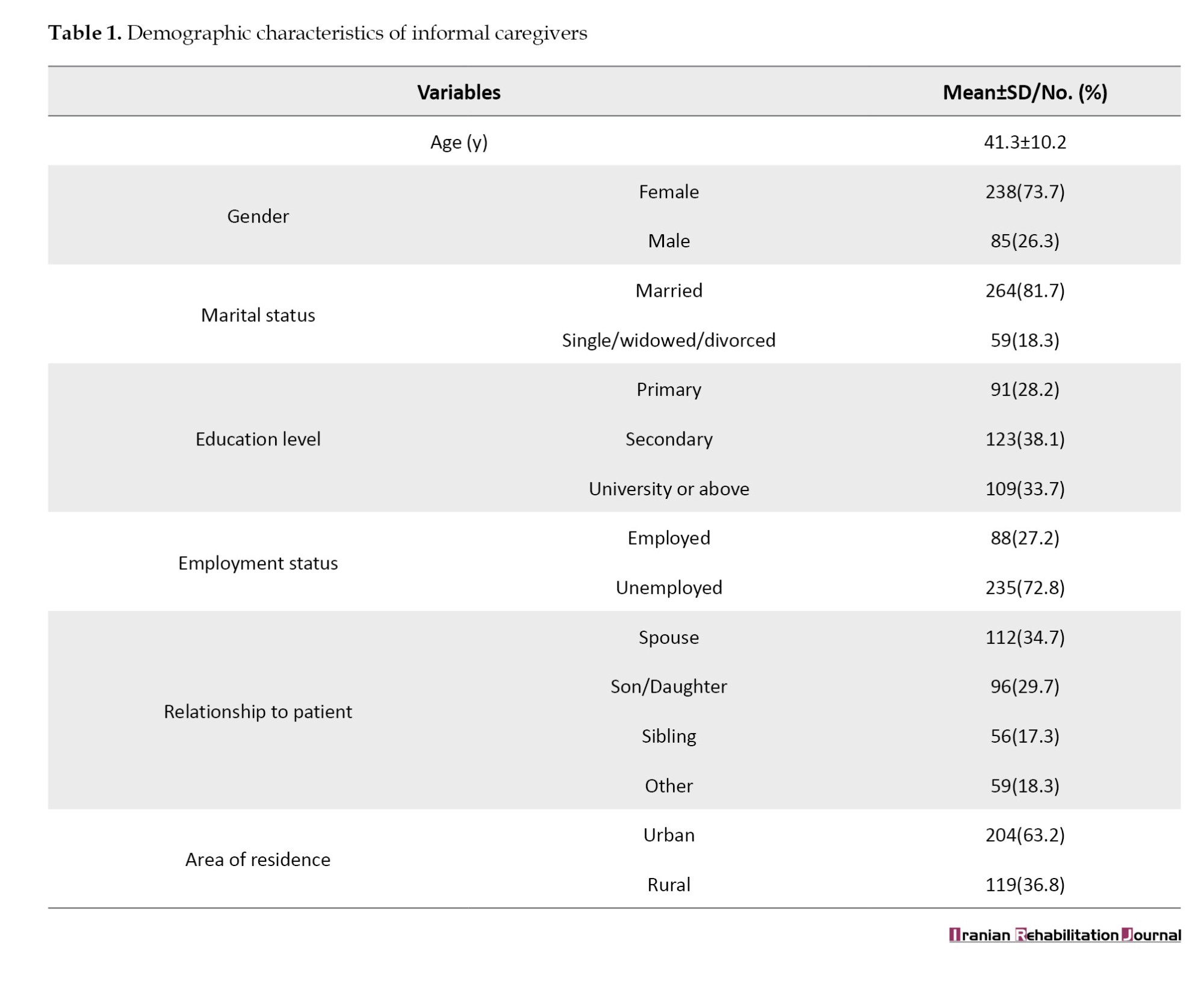
Table 2 presents the descriptive statistics for the ZBI-12, TUQ, and BI. The mean caregiver burden score (ZBI-12) was 25.6, suggesting moderate burden levels. The TUQ yielded a mean score of 112.3, indicating generally positive perceptions of telehealth. The BI averaged 61.4, reflecting a moderate level of functional independence among patients. The skewness and kurtosis values suggested that the data were approximately normally distributed, supporting parametric statistical analyses.
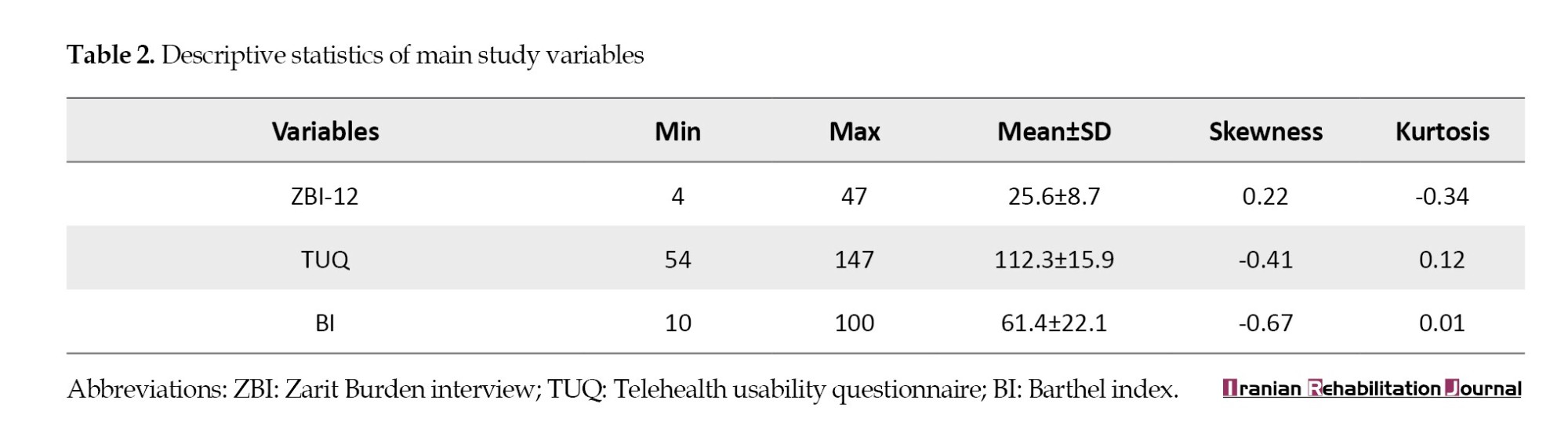
Table 3 presents significant correlations among the key study variables. Caregiver burden (ZBI) was negatively correlated with both telehealth usability (r=-0.63, P<0.01) and functional recovery (BI) (r=-0.71, P<0.01). Telehealth usability was positively correlated with functional recovery (r=0.66, P<0.01).

Table 4 presents the results of mediation analysis. All path coefficients were statistically significant. The indirect effect (a×b=-0.532) was significant (P<0.001), indicating partial mediation, suggesting that telehealth usability plays a role in the relationship between caregiver burden and functional recovery. The direct effect of caregiver burden on functional recovery (c′=-0.771) remained significant (P<0.001), implying that caregiver burden also independently influenced recovery outcomes.
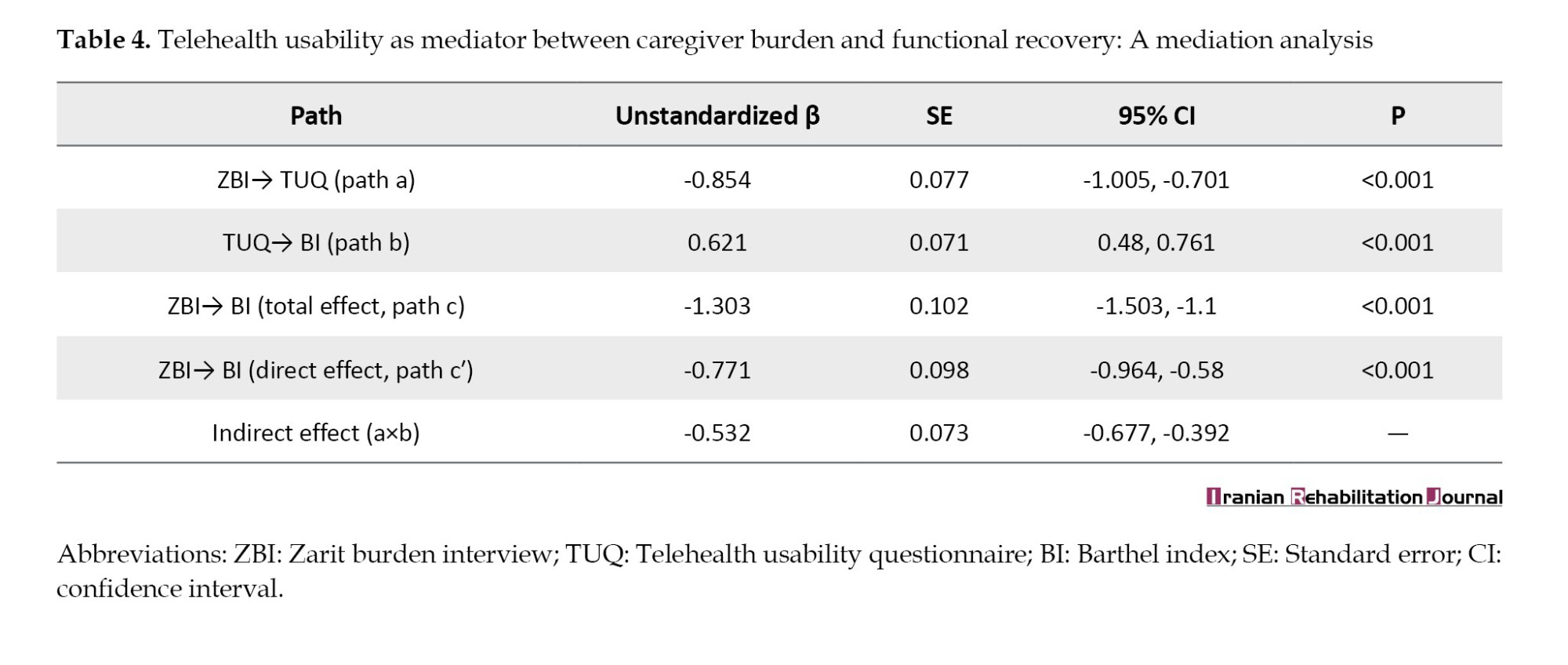
Table 5 presents the results of a multivariate linear regression predicting functional recovery (BI). Both caregiver burden (β=-0.62, P<0.001) and telehealth usability (β=0.55, P<0.001) were strong predictors of functional recovery. Higher education level was also a significant positive predictor (β=0.15, P=0.002). Caregiver age and area of residence were not significant predictors in this model. The overall model explained 57% of the variance in functional recovery (adjusted R²=0.56), indicating substantial predictive power.
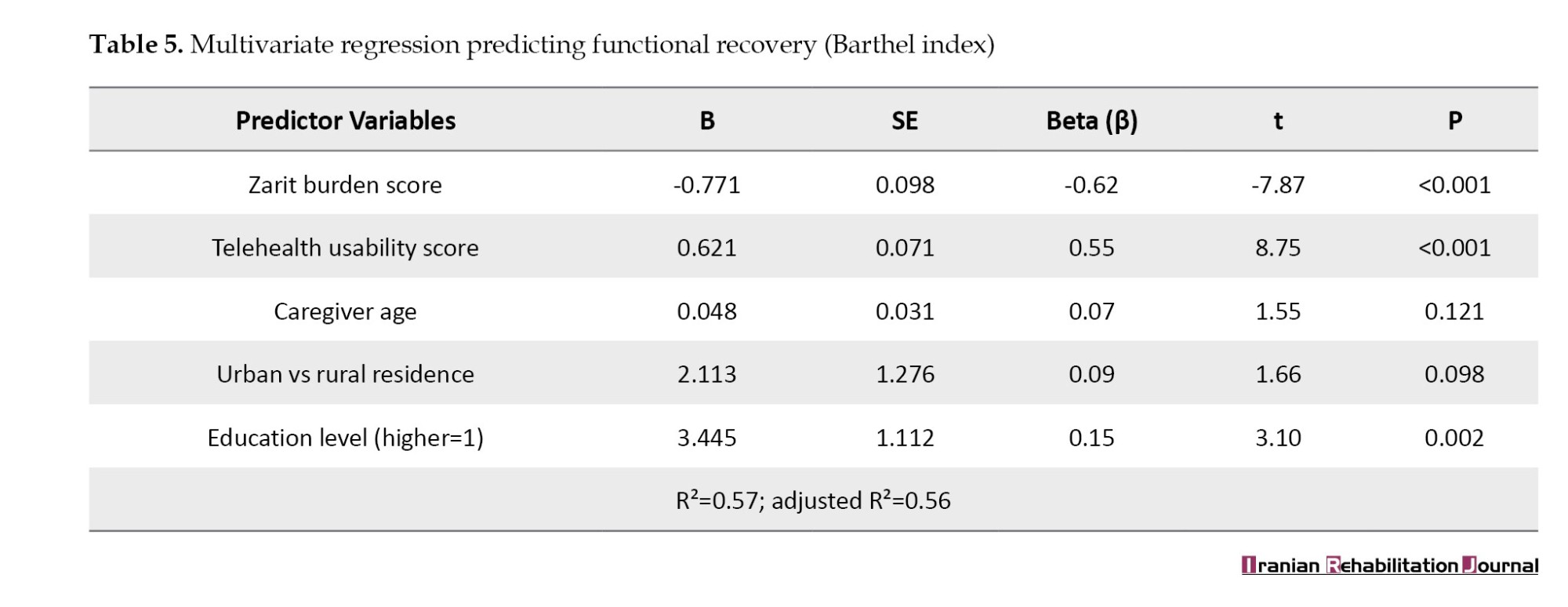
Table 6 compares the caregivers based on their areas of residence. Rural caregivers reported significantly higher burden (ZBI=28.2 vs 24.1, P<0.001), lower telehealth usability scores (107.1 vs 115.3, P<0.001), and their patients exhibited poorer functional recovery (BI=55.2 vs 64.8, P<0.001) compared to urban caregivers. These findings highlight disparities in caregiving experiences and outcomes based on geographic location.

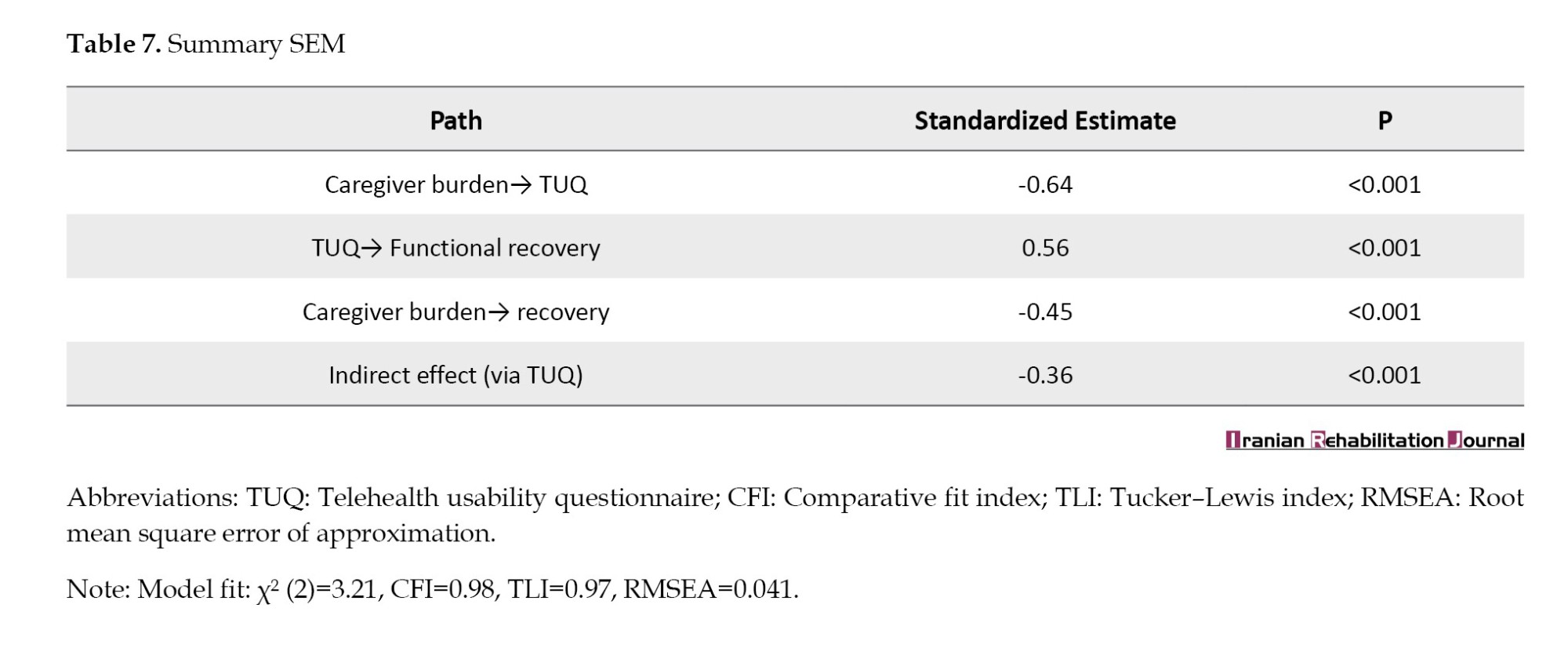
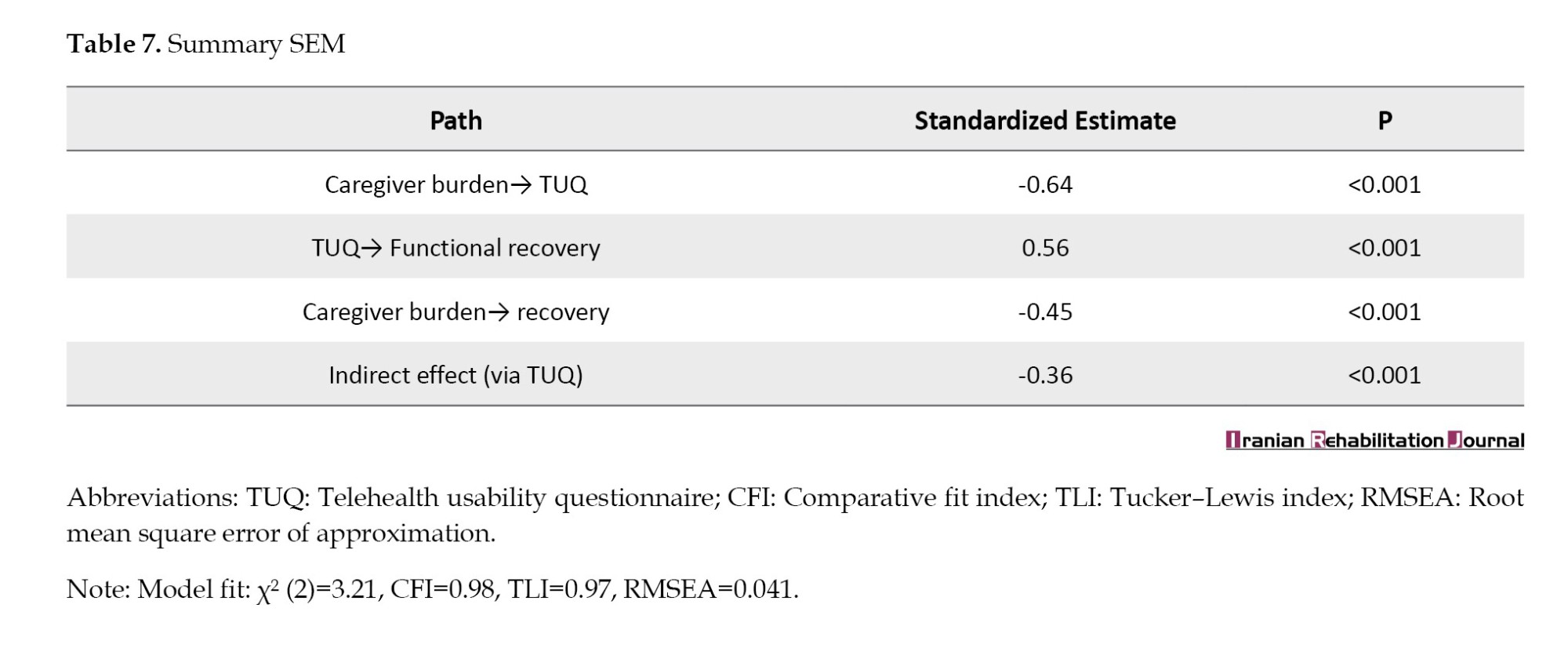
Table 7 presents the results of the structural equation modeling (SEM). The model indicated that caregiver burden had a significant negative direct effect on functional recovery (β=-0.45, P<0.001) and a significant negative indirect effect via telehealth usability (indirect β=-0.36, P<0.001). Telehealth usability positively influenced functional recovery (β=0.56, P<0.001), and caregiver burden negatively impacted telehealth usability (β=-0.64, P<0.001). The model fit indices (comparative fit index [CFI]=0.98, Tucker–Lewis index [TLI]=0.97, root mean square error of approximation [RMSEA]=0.041) suggest an excellent fit, supporting the proposed mediation framework.
Discussion
The descriptive analysis revealed moderate to high levels of perceived caregiver burden, mild telehealth usability, and impaired functional recovery in patients. The observed caregiver burden aligns with existing literature indicating significant mental and physical strain among informal caregivers in long-term care settings [6]. Moderate telehealth usability suggests the potential for enhancement of digital support systems. This finding is consistent with studies in similar populations where digital literacy and perceived value remain barriers to widespread telehealth adoption [17]. Lower BI scores reflect compromised functional independence, which is often associated with delayed rehabilitation outcomes, particularly when caregiver burden is high [18].
Significant negative correlations were found between caregiver burden, telehealth usability, and patient recovery. Conversely, a positive correlation was observed between telehealth usability and patient recovery. These relationships corroborate previous research demonstrating that elevated caregiver burden can negatively affect the utilization of supportive care and the quality of care provided, thereby hindering patient recovery [19]. Furthermore, the strong correlation between TUQ and BI underscores the critical role of user-friendly telehealth tools in facilitating functional recovery [20].
Mediation analysis indicated that telehealth usability significantly mediated the relationship between caregiver burden and patient recovery. The indirect effect (a×b=-0.532) suggests that a portion of caregiver burden’s impact on patient recovery is transmitted through the perceived usability of telehealth services. This finding is consistent with health technology implementation models that emphasize user perception as a determinant of effective intervention delivery [21]. It further highlights the potential of telehealth not only as a care delivery tool but also as a mediator capable of mitigating the adverse effects of caregiver strain on patient outcomes [22].
Regression analysis identified caregiver burden and telehealth usability as significant predictors of functional recovery, collectively explaining 56% of the variance (adjusted R2=0.56). Notably, caregiver age and residence location were not statistically significant predictors, whereas a higher education level showed a positive impact. This suggests that educational background may enhance caregivers’ capacity to navigate healthcare systems and engage with digital tools effectively, supporting the notion that education level correlates with greater health literacy and caregiving competence [23]. The strong negative beta coefficient for caregiver burden reinforces its status as a primary risk factor for patient progress [24, 25].
Urban caregivers reported significantly lower burden, higher telehealth usability, and better patient outcomes compared to their rural counterparts. This disparity likely reflects differences in digital infrastructure and healthcare access, consistent with research indicating that rural populations encounter barriers to telehealth, including limited connectivity, lower digital literacy, and less robust support infrastructure [26]. These findings imply that interventions to reduce caregiver burden and improve patient outcomes should be tailored to specific geographical and infrastructural contexts [27].
The SEM results supported the theoretical pathways: Caregiver burden negatively influenced telehealth usability and functional recovery, while telehealth usability positively impacted recovery. The model demonstrated robust fit indices, validating the hypothesized model and strengthening the argument that integrating technology-based interventions into caregiver support programs can reduce burden and enhance care outcomes. Prior SEM studies have established similar mediating effects of caregiver engagement and digital tools on health outcomes [28].
Empirical evidence from this study demonstrates that caregiver burden negatively impacts patient recovery, and the usability of telehealth services substantially mediates this relationship. These findings underscore the necessity for comprehensive digital support, tailored caregiver training, and health equity interventions, particularly for rural caregivers. In alignment with the technology acceptance and stress process models, these results highlight the interplay between psychosocial and technological factors in shaping patient recovery outcomes.
Conclusion
This study concluded that caregiver burden significantly hinders patient recovery, and this negative impact is partly attributable to the usability of telehealth systems. High caregiver burden was associated with lower telehealth usability and poorer patient recovery outcomes, particularly in rural areas with limited digital infrastructure. These findings emphasize the importance of supporting informal caregivers by addressing their psychosocial stressors and enhancing their proficiency in digital healthcare tools. Therefore, healthcare facilities should implement caregiver support programs that integrate digital literacy training, focusing on caregivers in underserved areas. Policymakers should prioritize investments in telehealth infrastructure and affordability to mitigate disparities in access and outcomes.
Study limitations
This study has several limitations. First, its cross-sectional design restricts establishing definitive causal relationships between caregiver burden, telehealth usability, and patient recovery. Second, data were collected via self-report questionnaires, susceptible to recall and social desirability biases. Third, the sample was drawn from a specific geographic region, potentially limiting the generalizability of the findings to other settings or populations. Finally, factors, such as Internet access quality and prior digital experiences were not controlled, which may have influenced telehealth usability outcomes.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethics Committee of the College of Nursing, University of Thi-Qar, Thi-Qar, Iraq (No.: 1213; Dated 2/3/2025). The Health Authority of Thi-Qar, Thi-Qar Health Directorate, Iraq, approved all experimental protocols, and all permitted guidelines were adhered to during the data collection.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, data collection and supervision: Salwan Abed Laftah; Writing the original draft: All authors; Data analysis, review, and editing: Asmaa Hammooz.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The Health Authority of Thi-Qar/ Thi-Qar Health Directorate, Iraq, approved all experimental protocols, and during the data collection, all permitted guidelines were adhered to.
References
Stroke remains a leading cause of long-term disability globally, frequently leaving survivors with significant physical, cognitive, and emotional impairments that necessitate continuous care [1]. Functional recovery in stroke patients is a complex process influenced by various factors, including exceptional post-discharge care and the pivotal role of informal caregivers [2]. Informal caregivers, typically family members, are instrumental in assisting stroke survivors through rehabilitation; however, they often experience excessive psychological, physical, and emotional burdens, which can negatively impact patient recovery outcomes [3, 4].
Recent research has consistently demonstrated a significant relationship between caregiver burden and functional recovery in stroke patients. Higher levels of burden are often linked to poorer patient outcomes, primarily due to reduced quality of care and increased caregiver burnout [5, 6]. Consequently, strategies aimed at alleviating caregiver burden and enhancing support mechanisms are crucial for improving patient recovery. One promising approach gaining increasing attention is the implementation of nurse-led telehealth interventions, which have proven effective in providing timely support, education, and monitoring for both patients and their caregivers [7, 8].
Nurse-led telehealth follow-up, typically encompassing remote consultations, health education, and ongoing monitoring by trained nurses, offers a valuable strategy to bridge existing gaps in post-discharge care [9, 10]. This approach not only enhances continuity of care but also empowers caregivers by offering guidance and emotional support, thereby potentially reducing their burden and positively influencing the patient’s rehabilitation [11, 12]. Furthermore, evidence suggests that such interventions improve self-management behaviors, medication adherence, and facilitate early detection of complications, all of which are critical for optimal stroke recovery [13].
Despite the growing body of literature supporting telehealth and caregiver support independently, there remains a notable gap in understanding the mediating role of nurse-led telehealth in the intricate relationship between caregiver burden and functional recovery in stroke patients. Exploring this mediating role is paramount for developing integrated care models and optimizing outcomes for both patients and caregivers. Therefore, this study aimed to investigate whether nurse-led telehealth follow-up can mediate caregiver burden and functional recovery among stroke patients.
Materials and Methods
Study design and setting
This study employed a cross-sectional, descriptive-correlational design. The primary objective was to examine the association between caregiver burden and functional recovery in patients with stroke, with a specific focus on the mediating role of network nurse-led telehealth follow-up. The research was conducted across multiple community-based rehabilitation facilities and outpatient neurology clinics affiliated with Al-Nasiriya Teaching Hospital, located in Thi-Qar Governorate, Iraq. The data collection period spanned from February 1st to June 30th, 2025. These specific healthcare settings were selected due to their established role in providing post-discharge rehabilitation and ongoing follow-up care for stroke survivors within the governorate. Their integration with community health nursing services and access to diverse patient populations made them ideal for gathering comprehensive data on caregiver experiences and patient recovery trajectories.
Study sample
A stratified random sampling method was utilized to ensure a representative sample of different types of informal caregivers for stroke survivors. Stratification was performed based on geographic area (urban vs rural) and type of healthcare facility (community health center vs outpatient clinic) to accurately reflect the region’s broader demographic and healthcare delivery patterns. The sample size was calculated using the formula for a single-population proportion. Based on an assumed incidence (p) of 30%, a 95% confidence level (Z=1.96), and a margin of error (d) of 0.05, the initial sample size (n₀) was determined to be 323. Considering the total eligible population of approximately 1200 stroke patients and their caregivers under follow-up, the final corrected sample size remained 323, ensuring adequate statistical power for the analyses.
Participants were eligible if they were 18 years or older, served as informal caregivers to a stroke patient discharged at least one month prior, and had participated in at least one network nurse-led telehealth follow-up session. Caregivers also required to understand Arabic sufficiently to provide informed consent and complete the study. Caregivers of patients with degenerative neurological conditions (Parkinson’s disease) or those with documented psychiatric illnesses that could impair their caregiving or response accuracy were excluded.
Study instruments
Three standardized and validated instruments were employed to collect data on the study variables:
Zarit burden interview-short version (ZBI-12)
This 12-item instrument measures caregivers’ perceived burden. Each item is rated on a 5-point Likert scale, ranging from 0 (never) to 4 (nearly always). The total score ranges from 0 to 48, with higher scores indicating greater caregiver burden. The Arabic version of the ZBI-12 has demonstrated robust internal consistency (Cronbach’s α=0.88) and good test re-test reliability (interclass correlation coefficient [ICC]=0.85) in Middle Eastern populations [13, 14].
Telehealth usability questionnaire (TUQ)
This 21-item scale assesses caregivers’ perceptions of the usability and effectiveness of telehealth services provided by community nurses. It covers multiple domains, including usefulness, ease of use, and interaction quality, with each item rated on a 7-point Likert scale. The Arabic version of the TUQ exhibited excellent psychometric properties in pilot testing (α=0.91, ICC=0.89), making it suitable for the study’s cultural and contextual settings [15].
Barthel index (BI)
The BI was used to assess the functional recovery of stroke patients, as reported by their caregivers. This 10-item instrument evaluates performance in basic activities of daily living, such as feeding, bathing, grooming, and mobility. The total score ranges from 0 (complete dependence) to 100 (complete independence). The Arabic version of the BI used in this study had been previously validated within the Iraqi healthcare system, and established studies show strong reliability (Cronbach’s α=0.95, ICC=0.93), confirming its widespread acceptance in stroke rehabilitation research [16].
Validity and reliability
To ensure cultural and linguistic appropriateness for the Iraqi context, all three instruments underwent a rigorous forward–backward translation process conducted by bilingual healthcare professionals experienced in both nursing and rehabilitation. The translated versions were subsequently reviewed by a panel of five academic and clinical experts in community health nursing to assess conceptual equivalence, readability, and content validity. A pilot study involving 30 caregivers (not included in the final sample) was conducted to test the instruments’ feasibility, readability, and internal consistency. The pilot results confirmed the suitability of these tools for the target population.
Data collection
Data were collected through self-administered questionnaires for literate participants and researcher-administered interviews for those with limited literacy. Data were collected in a private setting to ensure participant confidentiality. Trained data collectors with nursing backgrounds conducted the interviews in Arabic. Data collection occurred over four months (February 1st to June 30th, 2025) during routine outpatient rehabilitation or telehealth review clinic visits. Written informed consent was obtained from each participant prior to data collection. Ethical approval was obtained from the Scientific Research Ethics Committee of the College of Nursing, University of Thi-Qar. Participants were assured of confidentiality, voluntary participation, and their right to withdraw at any time without consequences to their care.
Data analysis
Data were analyzed using IBM SPSS software, version 26. Descriptive records, along with Mean±SD, frequencies, and probabilities, were used to summarize caregivers’ demographic traits, clinical data of stroke patients, and the total scores obtained from the ZBI, TUQ, and BI. The normality of continuous variables was assessed using the Kolmogorov-Smirnov and Shapiro-Wilk tests, along with visual inspection of histograms and assessment of skewness and kurtosis values. To examine the relationships among the primary study variables, Pearson’s correlation coefficient (r) was employed to determine the strength and direction of the bivariate associations among caregiver burden, telehealth observation usability, and functional recovery of stroke patients. Mediation analysis was performed using Hayes’ PROCESS macro (model 4) to assess the mediating role of community nurse-led telehealth follow-up (TUQ) in the relationship between caregiver burden (ZBI) and functional recovery (BI). The indirect effect was tested using a bootstrapping approach with 5,000 resamples to generate bias-corrected 95% confidence intervals (CI). Mediation was statistically significant when the confidence interval did not include zero. A P<0.05 was the threshold for statistical significance in some analyses.
Results
Table 1 presents the demographic characteristics of the informal caregivers. The Mean±SD age of the caregivers was 41.3±10.2 years. Most caregivers were female (73.7%) and married (81.7%). Educational attainment varied, with 38.1% having completed secondary education and 33.7% holding a university degree or higher. A significant portion (72.8%) was unemployed, potentially reflecting the demands of caregiving. The most common relationship to the patient was spouse (34.7%) and child (29.7%). Geographically, most caregivers resided in urban areas (63.2%).
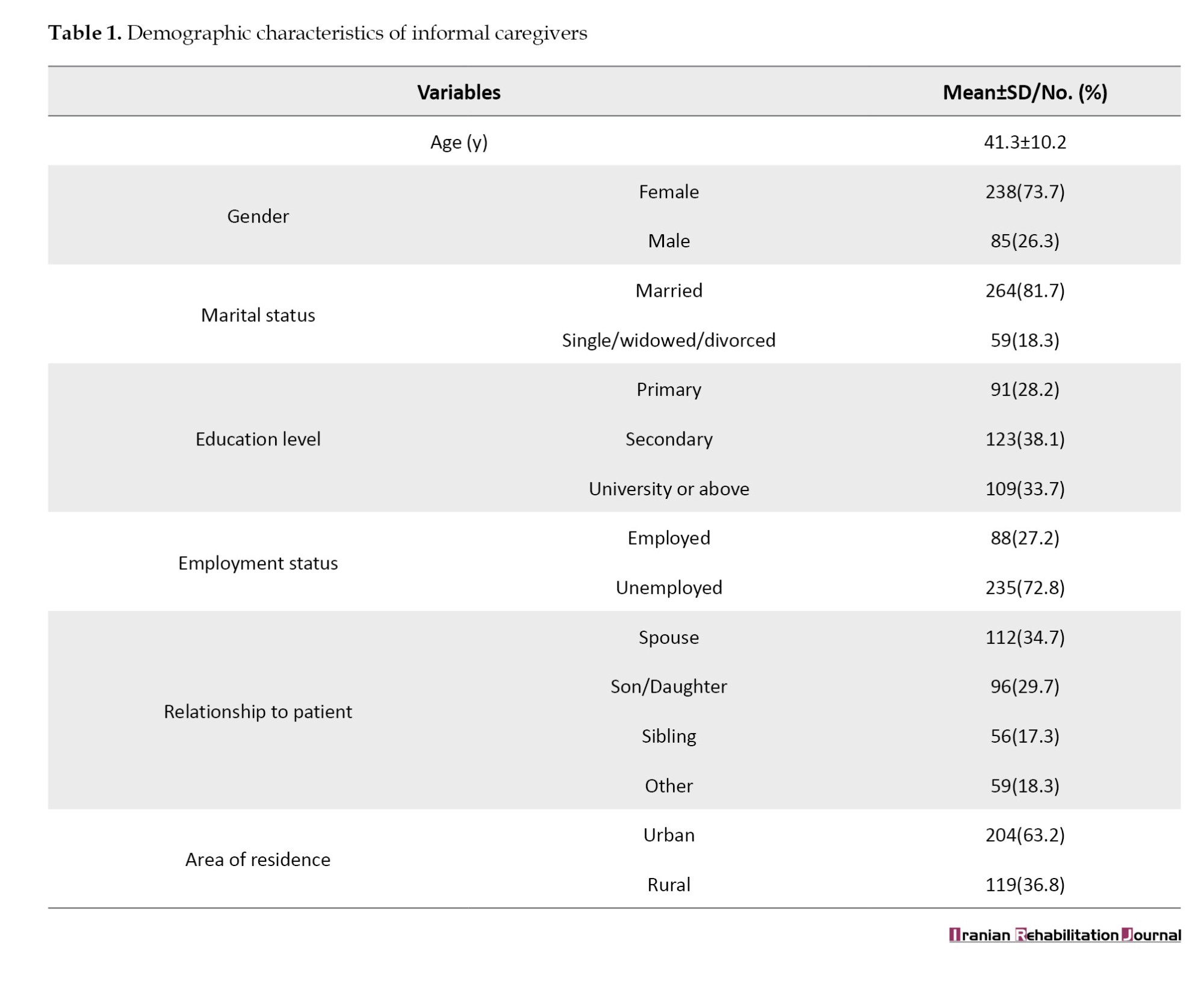
Table 2 presents the descriptive statistics for the ZBI-12, TUQ, and BI. The mean caregiver burden score (ZBI-12) was 25.6, suggesting moderate burden levels. The TUQ yielded a mean score of 112.3, indicating generally positive perceptions of telehealth. The BI averaged 61.4, reflecting a moderate level of functional independence among patients. The skewness and kurtosis values suggested that the data were approximately normally distributed, supporting parametric statistical analyses.
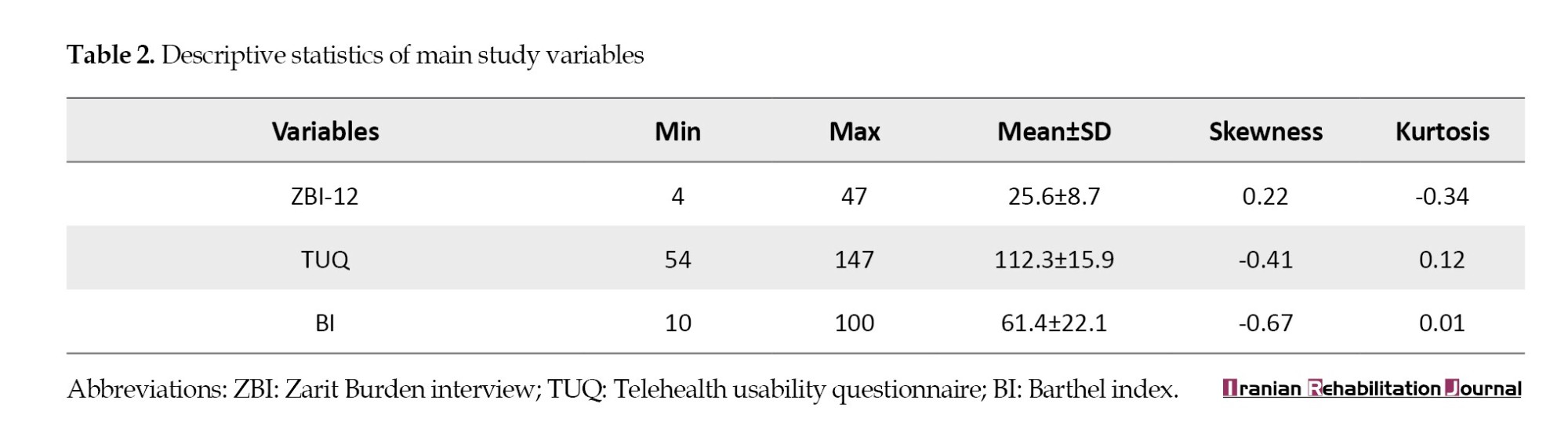
Table 3 presents significant correlations among the key study variables. Caregiver burden (ZBI) was negatively correlated with both telehealth usability (r=-0.63, P<0.01) and functional recovery (BI) (r=-0.71, P<0.01). Telehealth usability was positively correlated with functional recovery (r=0.66, P<0.01).

Table 4 presents the results of mediation analysis. All path coefficients were statistically significant. The indirect effect (a×b=-0.532) was significant (P<0.001), indicating partial mediation, suggesting that telehealth usability plays a role in the relationship between caregiver burden and functional recovery. The direct effect of caregiver burden on functional recovery (c′=-0.771) remained significant (P<0.001), implying that caregiver burden also independently influenced recovery outcomes.
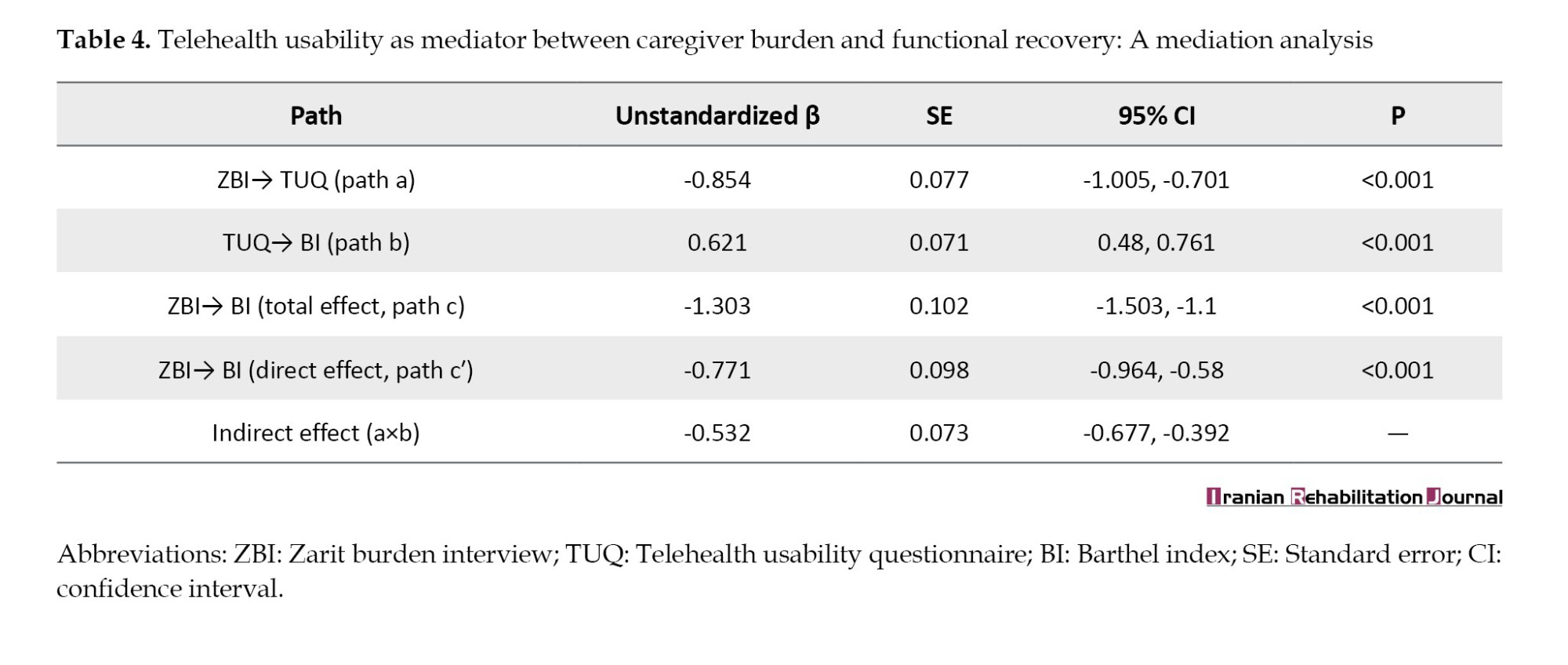
Table 5 presents the results of a multivariate linear regression predicting functional recovery (BI). Both caregiver burden (β=-0.62, P<0.001) and telehealth usability (β=0.55, P<0.001) were strong predictors of functional recovery. Higher education level was also a significant positive predictor (β=0.15, P=0.002). Caregiver age and area of residence were not significant predictors in this model. The overall model explained 57% of the variance in functional recovery (adjusted R²=0.56), indicating substantial predictive power.
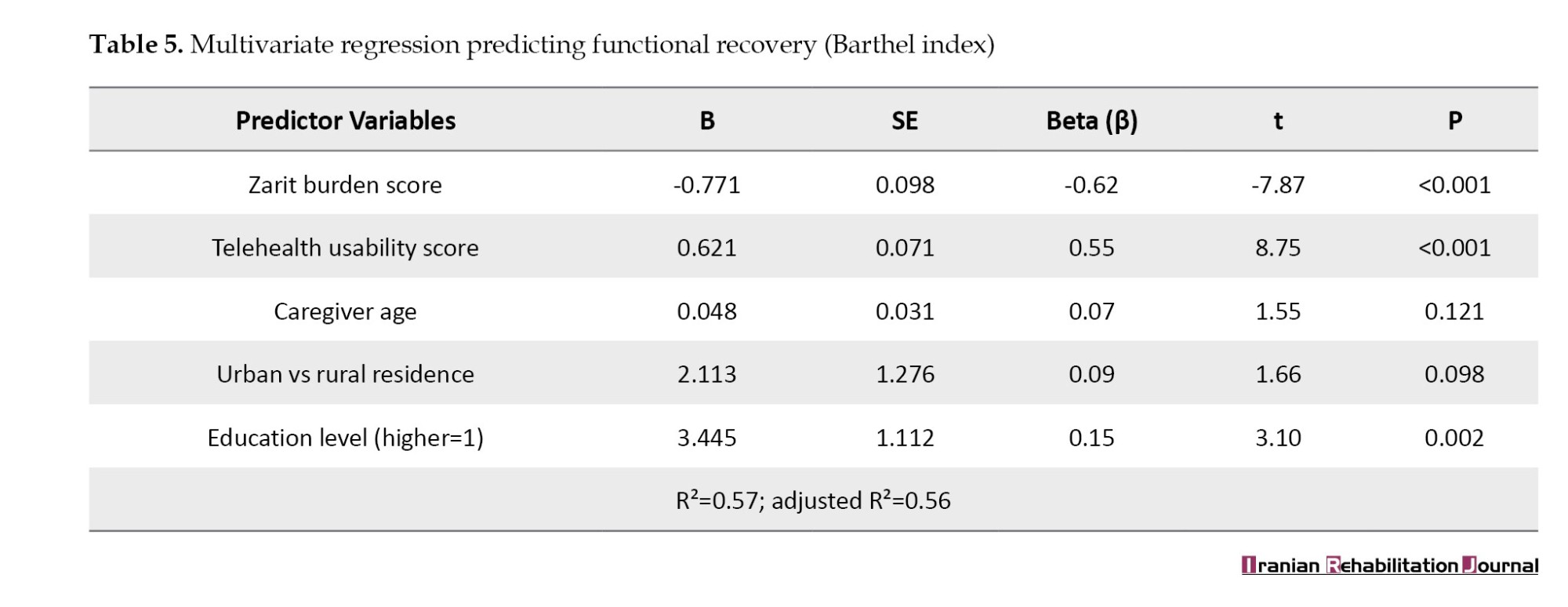
Table 6 compares the caregivers based on their areas of residence. Rural caregivers reported significantly higher burden (ZBI=28.2 vs 24.1, P<0.001), lower telehealth usability scores (107.1 vs 115.3, P<0.001), and their patients exhibited poorer functional recovery (BI=55.2 vs 64.8, P<0.001) compared to urban caregivers. These findings highlight disparities in caregiving experiences and outcomes based on geographic location.

Table 7 presents the results of the structural equation modeling (SEM). The model indicated that caregiver burden had a significant negative direct effect on functional recovery (β=-0.45, P<0.001) and a significant negative indirect effect via telehealth usability (indirect β=-0.36, P<0.001). Telehealth usability positively influenced functional recovery (β=0.56, P<0.001), and caregiver burden negatively impacted telehealth usability (β=-0.64, P<0.001). The model fit indices (comparative fit index [CFI]=0.98, Tucker–Lewis index [TLI]=0.97, root mean square error of approximation [RMSEA]=0.041) suggest an excellent fit, supporting the proposed mediation framework.
Discussion
The descriptive analysis revealed moderate to high levels of perceived caregiver burden, mild telehealth usability, and impaired functional recovery in patients. The observed caregiver burden aligns with existing literature indicating significant mental and physical strain among informal caregivers in long-term care settings [6]. Moderate telehealth usability suggests the potential for enhancement of digital support systems. This finding is consistent with studies in similar populations where digital literacy and perceived value remain barriers to widespread telehealth adoption [17]. Lower BI scores reflect compromised functional independence, which is often associated with delayed rehabilitation outcomes, particularly when caregiver burden is high [18].
Significant negative correlations were found between caregiver burden, telehealth usability, and patient recovery. Conversely, a positive correlation was observed between telehealth usability and patient recovery. These relationships corroborate previous research demonstrating that elevated caregiver burden can negatively affect the utilization of supportive care and the quality of care provided, thereby hindering patient recovery [19]. Furthermore, the strong correlation between TUQ and BI underscores the critical role of user-friendly telehealth tools in facilitating functional recovery [20].
Mediation analysis indicated that telehealth usability significantly mediated the relationship between caregiver burden and patient recovery. The indirect effect (a×b=-0.532) suggests that a portion of caregiver burden’s impact on patient recovery is transmitted through the perceived usability of telehealth services. This finding is consistent with health technology implementation models that emphasize user perception as a determinant of effective intervention delivery [21]. It further highlights the potential of telehealth not only as a care delivery tool but also as a mediator capable of mitigating the adverse effects of caregiver strain on patient outcomes [22].
Regression analysis identified caregiver burden and telehealth usability as significant predictors of functional recovery, collectively explaining 56% of the variance (adjusted R2=0.56). Notably, caregiver age and residence location were not statistically significant predictors, whereas a higher education level showed a positive impact. This suggests that educational background may enhance caregivers’ capacity to navigate healthcare systems and engage with digital tools effectively, supporting the notion that education level correlates with greater health literacy and caregiving competence [23]. The strong negative beta coefficient for caregiver burden reinforces its status as a primary risk factor for patient progress [24, 25].
Urban caregivers reported significantly lower burden, higher telehealth usability, and better patient outcomes compared to their rural counterparts. This disparity likely reflects differences in digital infrastructure and healthcare access, consistent with research indicating that rural populations encounter barriers to telehealth, including limited connectivity, lower digital literacy, and less robust support infrastructure [26]. These findings imply that interventions to reduce caregiver burden and improve patient outcomes should be tailored to specific geographical and infrastructural contexts [27].
The SEM results supported the theoretical pathways: Caregiver burden negatively influenced telehealth usability and functional recovery, while telehealth usability positively impacted recovery. The model demonstrated robust fit indices, validating the hypothesized model and strengthening the argument that integrating technology-based interventions into caregiver support programs can reduce burden and enhance care outcomes. Prior SEM studies have established similar mediating effects of caregiver engagement and digital tools on health outcomes [28].
Empirical evidence from this study demonstrates that caregiver burden negatively impacts patient recovery, and the usability of telehealth services substantially mediates this relationship. These findings underscore the necessity for comprehensive digital support, tailored caregiver training, and health equity interventions, particularly for rural caregivers. In alignment with the technology acceptance and stress process models, these results highlight the interplay between psychosocial and technological factors in shaping patient recovery outcomes.
Conclusion
This study concluded that caregiver burden significantly hinders patient recovery, and this negative impact is partly attributable to the usability of telehealth systems. High caregiver burden was associated with lower telehealth usability and poorer patient recovery outcomes, particularly in rural areas with limited digital infrastructure. These findings emphasize the importance of supporting informal caregivers by addressing their psychosocial stressors and enhancing their proficiency in digital healthcare tools. Therefore, healthcare facilities should implement caregiver support programs that integrate digital literacy training, focusing on caregivers in underserved areas. Policymakers should prioritize investments in telehealth infrastructure and affordability to mitigate disparities in access and outcomes.
Study limitations
This study has several limitations. First, its cross-sectional design restricts establishing definitive causal relationships between caregiver burden, telehealth usability, and patient recovery. Second, data were collected via self-report questionnaires, susceptible to recall and social desirability biases. Third, the sample was drawn from a specific geographic region, potentially limiting the generalizability of the findings to other settings or populations. Finally, factors, such as Internet access quality and prior digital experiences were not controlled, which may have influenced telehealth usability outcomes.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethics Committee of the College of Nursing, University of Thi-Qar, Thi-Qar, Iraq (No.: 1213; Dated 2/3/2025). The Health Authority of Thi-Qar, Thi-Qar Health Directorate, Iraq, approved all experimental protocols, and all permitted guidelines were adhered to during the data collection.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, data collection and supervision: Salwan Abed Laftah; Writing the original draft: All authors; Data analysis, review, and editing: Asmaa Hammooz.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The Health Authority of Thi-Qar/ Thi-Qar Health Directorate, Iraq, approved all experimental protocols, and during the data collection, all permitted guidelines were adhered to.
References
- El Husseini N, Katzan IL, Rost NS, Blake ML, Byun E, Pendlebury ST, et al. Cognitive impairment after ischemic and hemorrhagic stroke: A scientific statement from the American Heart Association/American Stroke Association. Stroke. 2023; 54(6):e272-91. [DOI:10.1161/STR.0000000000000430]
- van Dijk M, Vreven J, Deschodt M, Verheyden G, Tournoy J, Flamaing J. Can in-hospital or post discharge caregiver involvement increase functional performance of older patients? A systematic review. BMC Geriatrics. 2020; 20(1):362. [DOI:10.1186/s12877-020-01769-4] [PMID]
- Tziaka E, Tsiakiri A, Vlotinou P, Christidi F, Tsiptsios D, Aggelousis N, et al. A Holistic Approach to expressing the burden of caregivers for stroke survivors: A systematic review. Healthcare. 2024; 12(5):565. [DOI:10.3390/healthcare12050565] [PMID]
- Al-Eqabi QA, Niazy SM, Radhi MM. Amputation-related factors influencing activities of daily living among amputees. Iranian Journal of War and Public Health. 2024; 16(2):123-9. [DOI:10.58209/ijwph.16.2.123]
- Malih Radhi M, Zair Balat K. Health literacy and its association with medication adherence in patients with hypertension: A mediating role of social support. Iranian Rehabilitation Journal. 2024; 22(1):117-28. [DOI:10.32598/irj.22.1.1989.1]
- Malih Radhi M, Juma Elywy G, Abbas Khyoosh Al-Eqabi Q. Burdens among wives of disabled people in the light of some social variables. Iranian Rehabilitation Journal. 2023; 21(3):473-84. [DOI:10.32598/irj.21.3.1765.3]
- Radhi MM, Niazy SM, Abed SN. Individual-related factors associated with treatment adherence among hypertensive patients. Journal of Public Health in Africa. 2023; 14(6):2466. [DOI:10.4081/jphia.2023.2466] [PMID]
- Radhi MM, Al-Eqabi QA, Hindi NK. Rehabilitation problems of people with motor disabilities at Babylon center for rehabilitation of the disabled. Medical Journal of Babylon. 2023; 20(4):838-43. [DOI:10.4103/MJBL.MJBL_674_23]
- Davis K, Ramsey I, Sharplin G, Eckert M, Shakib S. A nurse-led, telehealth transitional care intervention for people with multimorbidity: A feasibility study. The Australian Journal of Advanced Nursing. 2024; 41(4):43-52. [DOI:10.37464/2024.414.1843]
- Radhi MM. Degree of disease acceptance and health seeking behaviors for type 2 diabetic patients at diabetic center in Hilla City. Medico-Legal Update. 2020; 20(2):853-. [DOI:10.37506/mlu.v20i2.1347]
- Pedrosa AR, Ferreira ÓR, Baixinho CR. Transitional rehabilitation care and patient care continuity as an advanced nursing practice. Revista Brasileira de Enfermagem. 2022; 75:e20210399. [DOI:10.1590/0034-7167-2021-0399] [PMID]
- Chen L, Xiao LD, Chamberlain D, Newman P. Enablers and barriers in hospital‐to‐home transitional care for stroke survivors and caregivers: A systematic review. Journal of Clinical Nursing. 2021; 30(19-20):2786-807. [DOI:10.1111/jocn.15807] [PMID]
- Sahely A, Giles D, Sintler C, Soundy A, Rosewilliam S. Self-management interventions to improve mobility after stroke: An integrative review. Disability and Rehabilitation. 2023; 45(1):9-26. [DOI:10.1080/09638288.2022.2028019] [PMID]
- Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: Correlates of feelings of burden. The Gerontologist. 1980; 20(6):649-55. [DOI:10.1093/geront/20.6.649] [PMID]
- Parmanto B, Allen Nelson Lewis JR, Graham KM, Bertolet MH. Development of the telehealth usability questionnaire (TUQ). International Journal of Telerehabilitation. 2016; 8(1):3. [DOI:10.5195/ijt.2016.6196] [PMID]
- Fi M. Functional evaluation: the Barthel index. Maryland State Medical Journal. 1965; 14:61-5. [Link]
- Kruse C, Fohn J, Wilson N, Patlan EN, Zipp S, Mileski M. Utilization barriers and medical outcomes commensurate with the use of telehealth among older adults: Systematic review. JMIr Medical Informatics. 2020; 8(8):e20359. [DOI:10.2196/20359] [PMID]
- Perez Marmol JM, Flores Antigüedad ML, Castro Sanchez AM, Tapia Haro RM, García Ríos MD, Aguilar Ferrandiz ME. Inpatient dependency in activities of daily living predicts informal caregiver strain: A cross‐sectional study. Journal of Clinical Nursing. 2018; 27(1-2):e177-85. [DOI:10.1111/jocn.13900] [PMID]
- Maggio MG, Corallo F, De Francesco M, De Cola MC, De Luca R, Manuli A, et al. Understanding the family burden and caregiver role in stroke rehabilitation: Insights from a retrospective study. Neurological Sciences . 2024; 45(11):5347-53. [DOI:10.1007/s10072-024-07668-5] [PMID]
- Zimmermann J, Morf H, Scharf F, Knitza J, Moeller H, Muehlensiepen F, et al. German version of the telehealth usability questionnaire and derived short questionnaires for usability and perceived usefulness in health care assessment in telehealth and digital therapeutics: Instrument validation study. JMIR Human Factors. 2024; 11:e57771. [DOI:10.2196/57771] [PMID]
- Getachew E, Woldeamanuel Y, Manyazewal T. Digital health interventions in the clinical care and treatment of tuberculosis and hiv in central Ethiopia: An initial provider perceptions and acceptability study using the unified theory of acceptance and use of technology model. International Journal of Mycobacteriology. 2022; 11(1):1-9. [DOI:10.4103/ijmy.ijmy_235_21] [PMID]
- Alwatify SS, Radhi MM. Diabetes self-management and its association with medication adherence in diabetic patients. Iranian Journal of War and Public Health. 2025; 17(1):17-22. [DOI:10.58209/ijwph.17.1.17]
- Balat KZ, Laftah SA, Radhi M. The relationship between psychological distress and quality of life among women undergoing mastectomy in Iraq: A descriptive correlational study. National Journal of Community Medicine. 2025; 16(1):20-7. [DOI:10.55489/njcm.160120254716]
- Al-Eqabi QA, Niazy SM, Radhi MM. Effectiveness of digital health interventions in managing glycated haemoglobin: A randomized controlled trial. National Journal of Community Medicine. 2024; 15(9):747-53. [DOI:10.55489/njcm.150920244442]
- Qassim WJ, Yasir AA, Radhi MM. Assessment of self hardness and its relationship to treatment acceptance for patients with diabetes mellitus at diabetic center in Hilla City/Iraq. Journal of Pharmaceutical Sciences and Research. 2018; 10(1):142-5. [Link]
- Elywy GJ, Radhi MM, AlEqabi QA. Relationship between social support and self-hardiness among breast cancer women in Nasiriyah, Iraq. Journal of the Pakistan Medical Association. 2023; 73(9):S9-14. [DOI:10.47391/JPMA.IQ-02]
- Juma Elywy G, Radhi MM, Khyoosh Al-Eqabi QA. Social support and its association with the quality of life (qol) of amputees. Iranian Rehabilitation Journal. 2022; 20(2):253-60. [DOI:10.32598/irj.20.2.1784.1]
- Guntu M, Lin EJ, Sezgin E, Gregory ME, Huang Y, Linwood SL. Identifying the factors influencing patients’ telehealth visit satisfaction: Survey validation through a structural equation modeling approach. Telemedicine and e-Health. 2022; 28(9):1261-9. [DOI:10.1089/tmj.2021.0372] [PMID]
Article type: Original Research Articles |
Subject:
Nursing
Received: 2025/06/29 | Accepted: 2025/08/16 | Published: 2025/12/1
Received: 2025/06/29 | Accepted: 2025/08/16 | Published: 2025/12/1
Send email to the article author