Volume 22, Issue 2 (June 2024)
Iranian Rehabilitation Journal 2024, 22(2): 321-332 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Farooq Khaleel R, Basim Al Khafajy M. Investigating the Parented-reported Quality of Life in Young Children With Cerebral Palsy at Ages of 5 to 7 years. Iranian Rehabilitation Journal 2024; 22 (2) :321-332
URL: http://irj.uswr.ac.ir/article-1-1989-en.html
URL: http://irj.uswr.ac.ir/article-1-1989-en.html
1- Department of Physiotherapy, College of Health and Medical Technologies, Middle Technical University, Baghdad, Iraq.
2- Medical Rehabilitation and Rheumatology Center, Baghdad, Iraq.
2- Medical Rehabilitation and Rheumatology Center, Baghdad, Iraq.
Keywords: Parented, Cerebral palsy, Children, Health-related quality of life (QoL), Gross motor function classification system (GMFCS)
Full-Text [PDF 600 kb]
(949 Downloads)
| Abstract (HTML) (3220 Views)
Full-Text: (548 Views)
Introduction
Cerebral palsy (CP) is caused by non-progressive abnormalities in the growing brain of a fetus or child, resulting in movement and posture problems and activity limitations. In addition to motor impairments, CP patients often have sensory, cognitive, communicative, perceptual, and behavioral problems [1]. CP, one of the most common motor disabilities in childhood, is more common in boys than girls due to biological factors, such as a more vulnerable cerebral structure, hormone protective factors, and genetic polymorphism [2], with an estimated average of approximately 3.6 cases per 1000 individuals [3]. CP is a social problem facing society in general and the family in particular and is associated with a variety of social challenges for families and the community. The family may experience more stress because of the children’s need for personal care as well as medical support and protection. CP children have a reduced quality of life (QoL) due to mobility issues and lesser participation in recreational and social activities [4]. World Health Organization (WHO) refers to QoL as a person’s sense of self in light of their culture, value system, goals, expectations, and worries [5]. The perspectives of patients about health-related QoL have considerable importance. QoL evaluations are often used by professionals in the fields of physiotherapy, psychology and social work. The pediatric QoL inventory (PedsQLTM) is one method used tools to assess this aspect of health in young people, whether they are experiencing acute or chronic illness. The WHO suggests measuring a child’s physical, mental, social, and educational involvement using the PedsQLTM 3.0 generic core scales. The QoL of youngsters (aged 5-7 years) was assessed in this study. Recent attention has focused on CP children’s health and QoL. This research used health-related QoL and functional movements to predict social and emotional coping behaviors and the link between QoL and age, gender, and body mass index (BMI). The researchers also want to learn more about the links between the different types of CP categories and patients’ QoL.
Providing well-coordinated and high-quality services focused on their needs encourages social inclusion. It allows them and their families to continue living an everyday life in the community. As the incidence of CP among Iraqi children continues to rise, this study is the first to examine their QoL in Baghdad City, Iraq.
Materials and Methods
This cross-sectional research included CP youngsters and their parents. A pediatric neurologist identified 149 children with CP. They were selected using a nonprobability purposive sampling method from the patients attending the Medical Rehabilitation and Rheumatology Centre. The data were collected from August 2022 to February 2023. This research utilized the Arabic translation of the PedsQLTM 3.0 CP module [6]. Parental reporting for young children (ages 5-7 years) was used instead of a self-completion questionnaire due to intellectual disabilities and communication difficulties in these children [7]. In all patients, mothers completed questionnaires through direct interviews. We obtained a verbal agreement from all the participants. During this study, mothers completed a 35-item (7 domains) questionnaire on the PedsQLTM 3.0 CP module for each child, as well as providing some sociodemographic information about the mother and her health, diseases, or illnesses associated with pregnancy. Additionally, some information about the age, sex, weight, height, mood of delivery, and place of birth was gathered. The gross motor function classification system (GMFCS) for CP was used to categorize functional status according to motor activity. CP children were classified according to physiological and topographic characteristics.
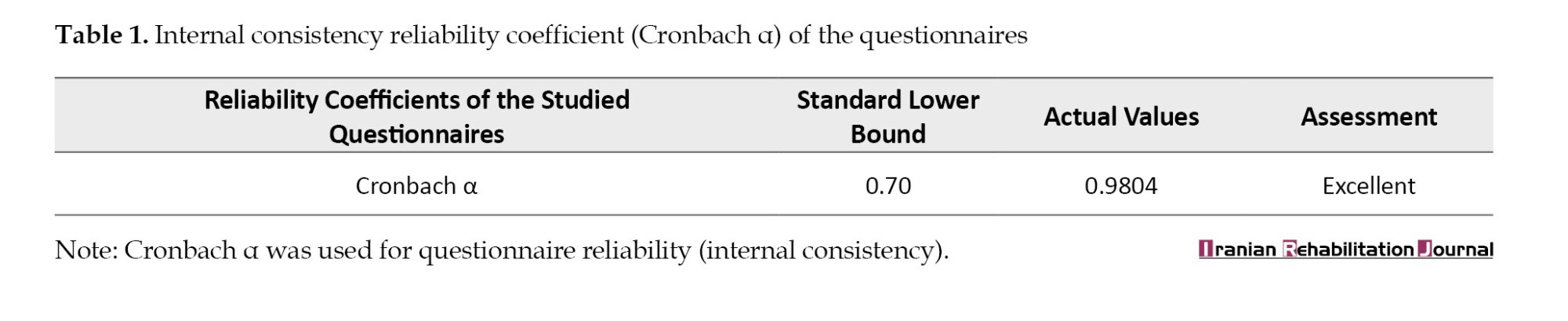
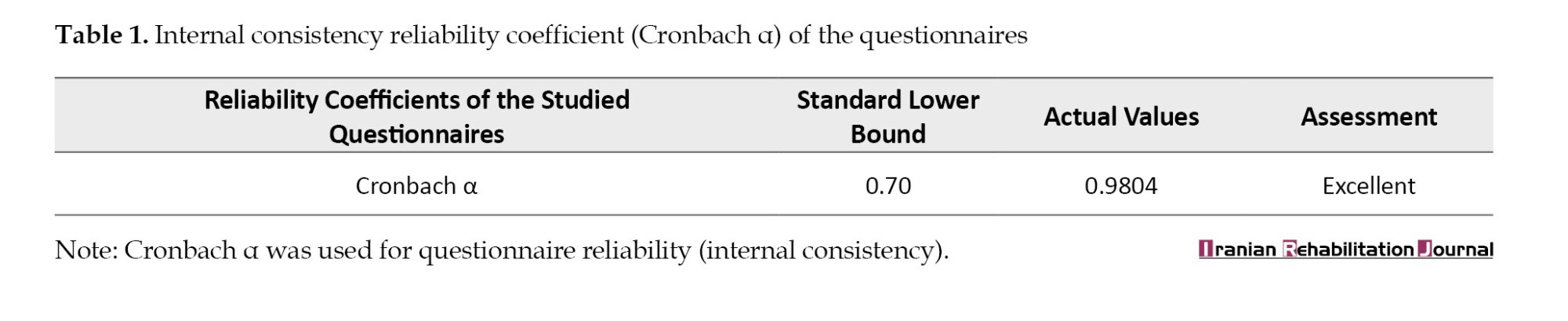
The Arabic iteration of the PedsQLTM 3.0 CP module comprises 35 items further categorized into 7 distinct domains. The framework encompasses several categories, including daily activities, school-related activities, mobility and balance, pain and injury management, weariness, eating activities and speech and communication skills. The scoring system ranges from 0 (indicating the absence of a problem) to 4 (indicating a high frequency of occurrence) as determined by the format, instructions, and the Likert answer scale. The 0-4 scale components are translated to 0-100 for better understanding. If over 50% of the items within the scale are absent, it is not advisable to calculate the scale scores. Meanwhile, higher scores on the scale indicate a greater QoL characterized by a reduced presence of symptoms or challenges. In this given numerical sequence, the values assigned to the numbers 0, 1, 2, 3 and 4 are 100, 75, 50, 25, and 0, respectively. A pilot study was conducted to verify the questionnaire’s reliability, and the final questionnaire was tested on 10 women, yielding the result=0.98, as shown in Table 1. A panel of 10 experts from diverse fields assessed the questionnaire’s validity.
As researchers, we excluded the school activities domain from questionnaire responses since most children involved in the study were not enrolled in schools due to a lack of awareness among parents of the possibility of educating their children, whether in a mainstream or a private school, for children with special needs. The data analyses were performed via the SPSS software, version 26. For categorical variables, descriptive statistics were provided as frequencies and percentages, while for continuous variables, the Mean±SD were determined. Furthermore, substantial comparisons were made to test the reliability of the random distribution hypothesis. The scores were computed based on the PedsQLTM manual. The Cronbach α coefficient was used to conduct reliability analyses based on the average correlation between items, and an interference analysis (contingency coefficient and chi-square) was also conducted to analyze data. The P≤0.05.
Results
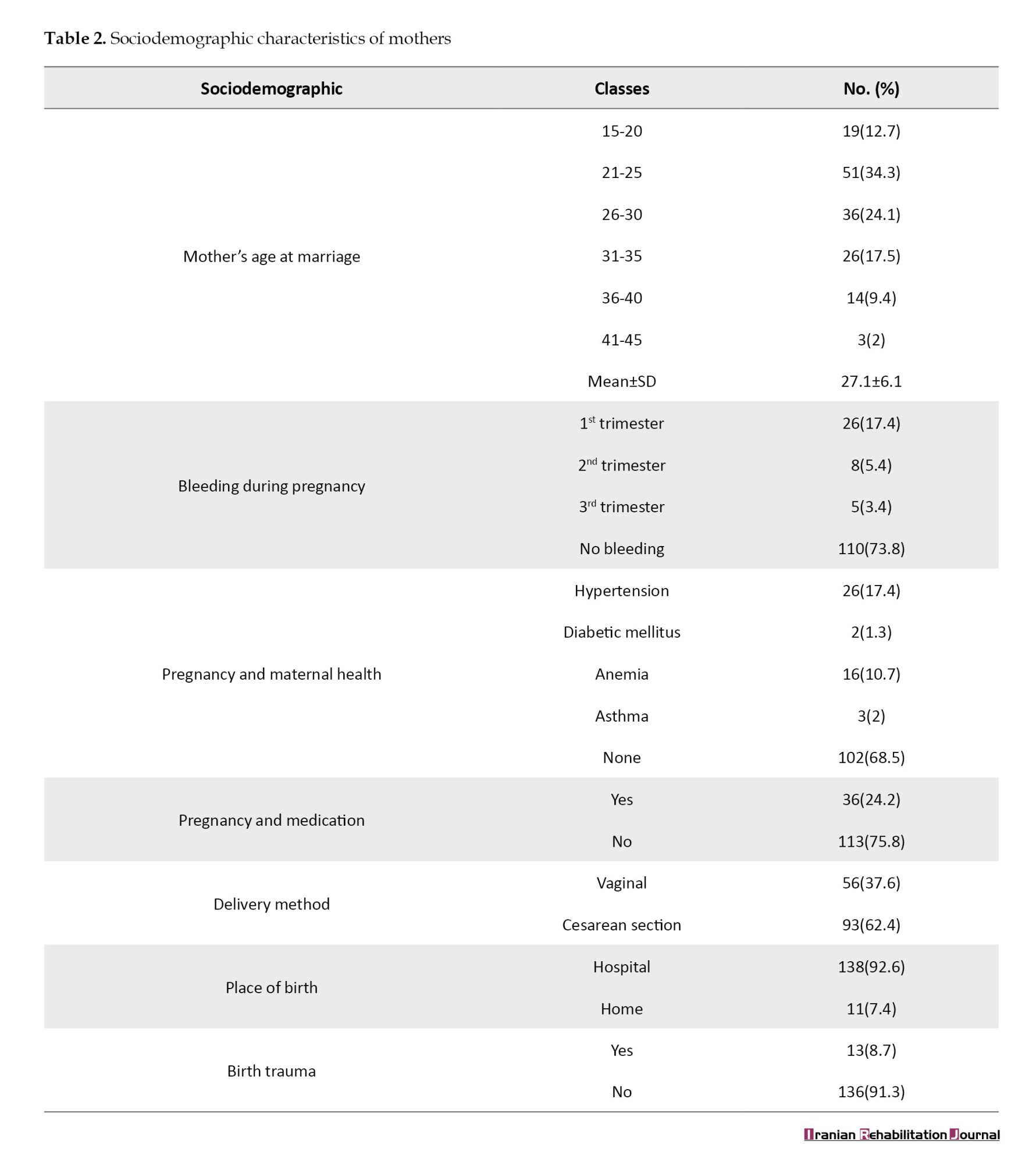
Data characteristics of mothers of children
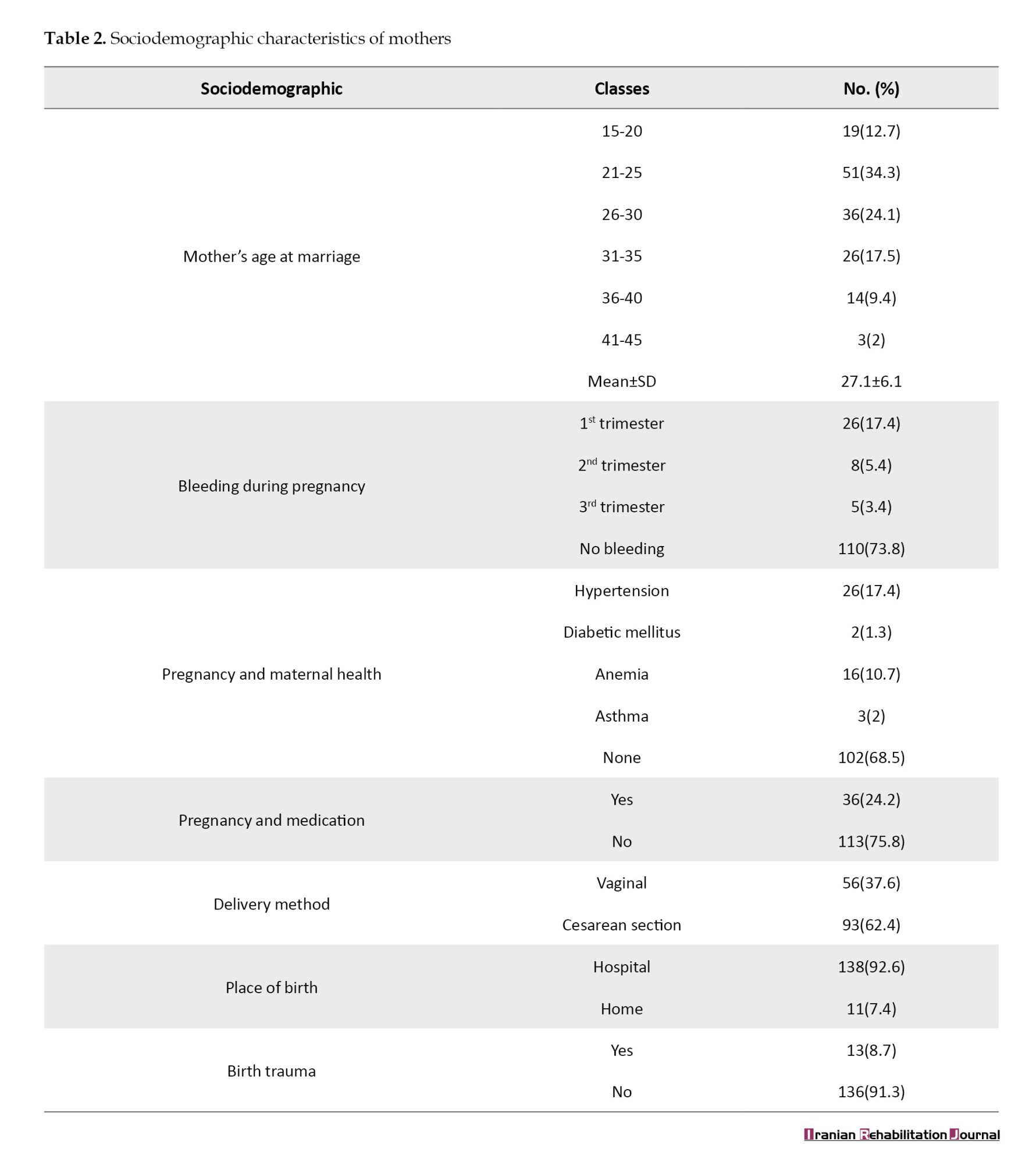
The characteristics of mothers and birth conditions related to CP in children are summarized in Table 2. More than a third, 51(34.3%), of the mothers married at the age between 21-25 years with a mean age of 27.1 years. In addition, over two-thirds, 110(73.8%) of those surveyed reported a normal pregnancy without bleeding. Maternal healthcare during pregnancy showed that more than two-thirds, 102(68.5%), of mothers are healthy, while a minority suffer from hypertension, anemia, asthma, and diabetes mellitus, respectively. While pregnant, the majority of mothers, 113(75.8%), did not take medication during pregnancy. In this study, 93 children (62.4%) were delivered via vaginal delivery and 56(37.6%) were delivered via cesarean section. Almost all the children, 138(92.6%) born in a hospital, and the minority of them, 13(8.7%), have been exposed to trauma at birth or throughout their first year of life.
Sociodemographic characteristics of CP children
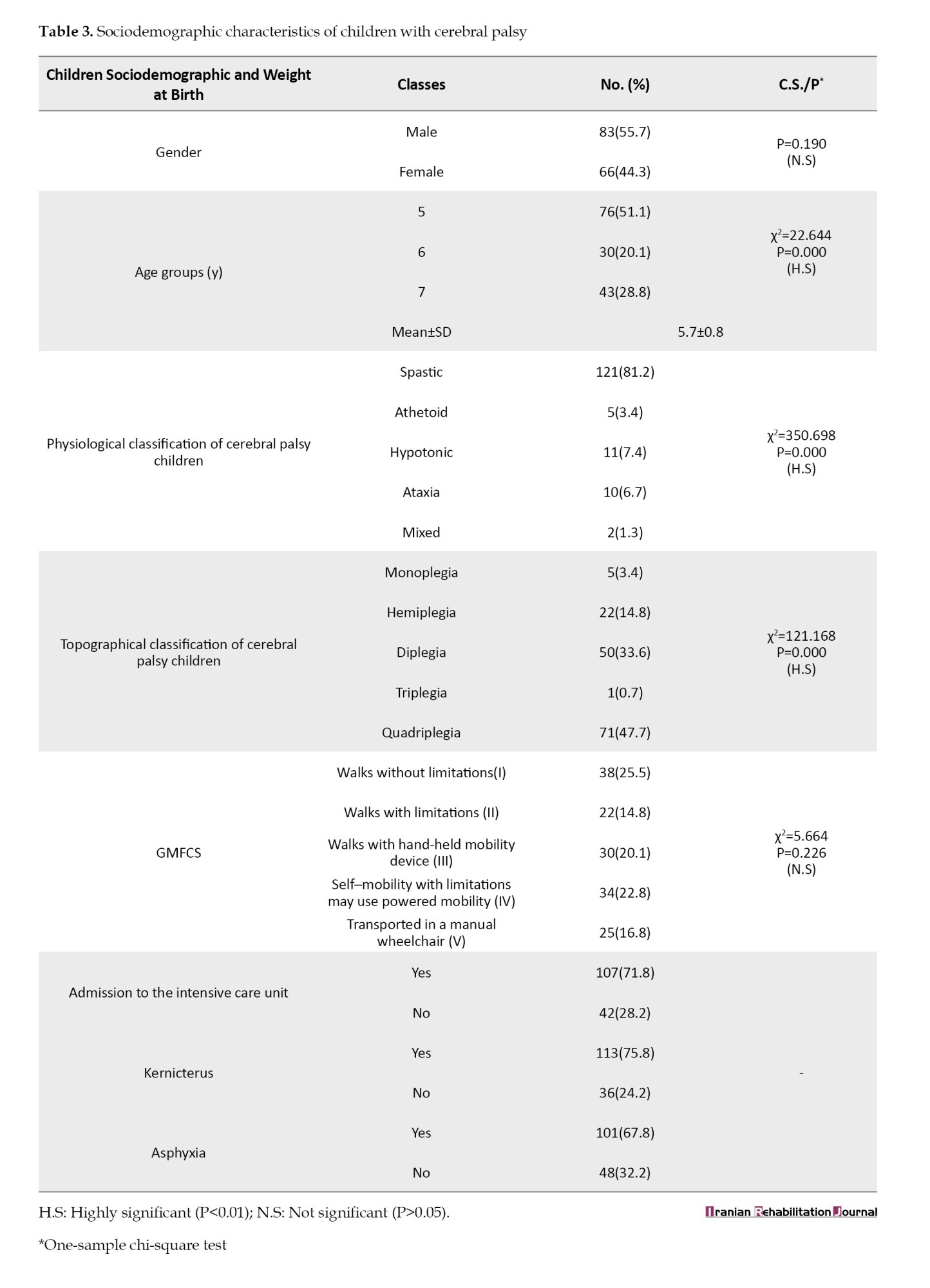
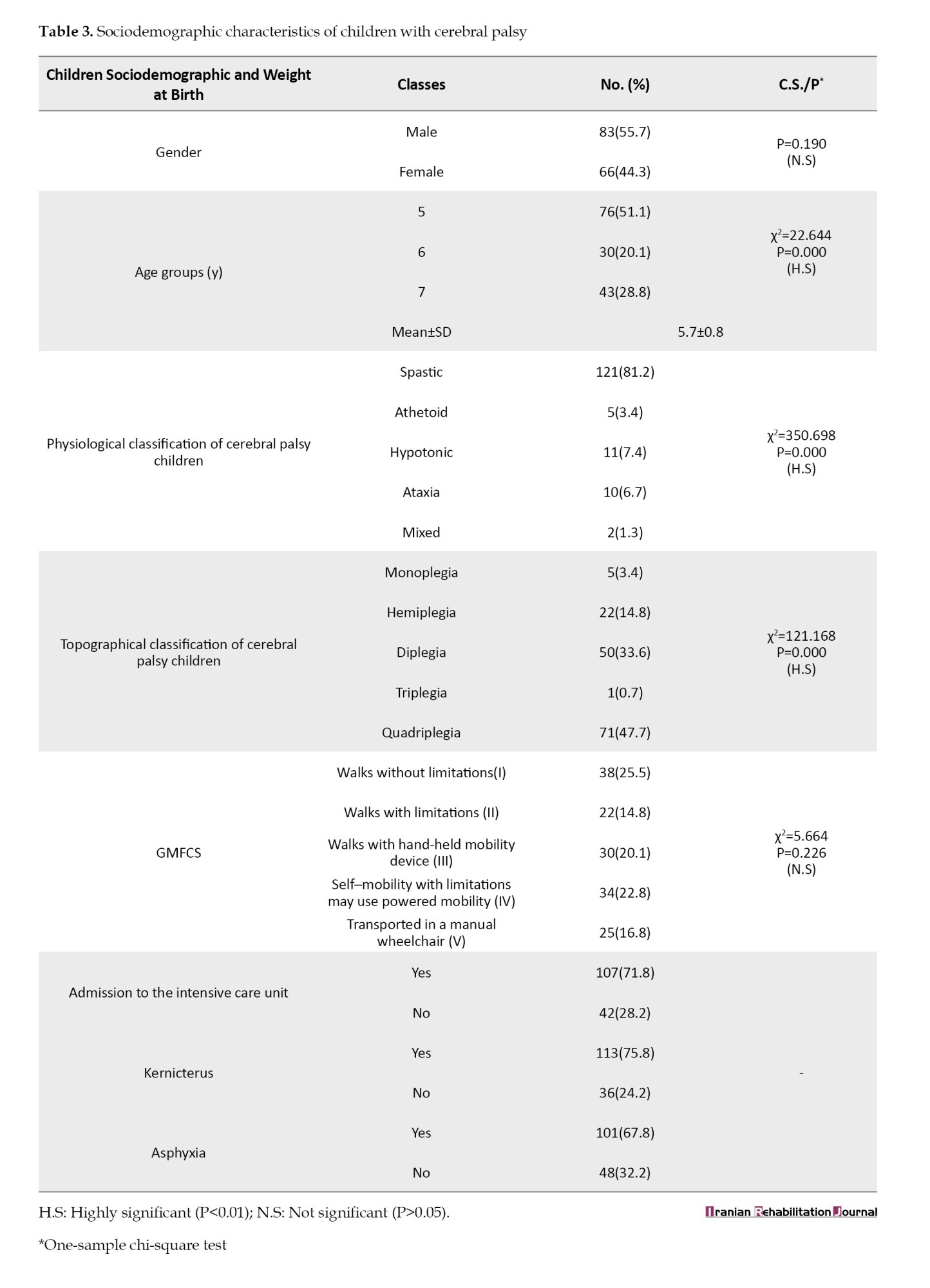
According to Table 3, This research included 149 CP patients, with an average age of 5.7±0.8 years, and 83(55.7%) of them were male. Most kids in the oldest age group of 5 years old were not in regular or special education programs, even though just over half of them (51.1%) were old enough to go to school. Nearly 48% of youngsters had quadriplegia and 81.2% of them had spastic CP. The GMFCS classified 38(25.5%) children as level I, followed by 34(22.8%) children as level IV. More than two-thirds of the study cohort (71.80%) had to be admitted to neonatal care facilities, according to our findings. Neonatal jaundice is a known risk factor for CP, and 113 patients (74.8%) in this research exhibited this symptom. Additionally, 101 patients (67.8%) reported experiencing birth asphyxia.
The data reported in Table 4 showed that about two-thirds of the studied sample were underweight (n=92, 61.7%), while 53 cases (36.6%) were registered as normal weight, and only 4(2.7%) were overweight. Among various BMI groups, there were highly significant variations (P=0.01). The preponderance of children with CP who were assessed are underweight, as supported by the results.

As with the parents of children with CP, QoL was assessed in six different areas. The evaluation did not include academic assignments but rather encompassed different aspects, such as everyday activities, physical coordination and stability, discomfort and discomfort, exhaustion, dietary habits, and verbal expression and communication. On a four-category scale with scores of (0, 1, 2, 3 and 4), “never,” “always,” “never,” “sometimes,” “often” and “almost always” were assigned to each area. Table 5 summarizes the initial assessment statistics, including Mean±SD score, and relative adequacy. Scores are categorized into three levels low, medium, and high, depending on their transferred scores and their relative adequacy intervals ([0.00-33.33], [33.34-66.66], [66.67-100]).

Based on the results of Table 5, seven items within the domain of daily activities are evaluated at a moderate level (77.78%) and 2 items at a high level (22.22%). In the movement and balance domain, 3(60.0%) items are evaluated at a moderate level and 1(20.0) item is evaluated at a high and low level. In the response to the pain and aches domain, 3(60.0%) items are rated moderately, 1(20.0) item is rated high, and 1(20.0) item is rated low. In the fatigue domain, all items are rated low. Meanwhile, in the eating activities domain, 3(60%) items rated moderate level and 2(40%) items at a low level. Lastly, in the speech and communicate domain, 2(50%) items were rated low, and 2(50%) items were rated moderate. According to the findings of prior research, the QoL of the parents was shown to have a negative correlation with the health-related QoL of their CP children. This association was mostly the result of the research having a mediocre to bad evaluation of the majority of the items.
The PedsQLTM 3.0 CP module’s first findings were obtained through parents’ reports. These findings are provided in Table 6, which includes the percentile grand mean score, pooled standard deviation and reliability for each subscale. The consistency of the results across all of the subscales was used to evaluate the dependability of the measurements. The Cronbach α coefficient of 0.905 indicates that the PedsQLTM scale exhibited excellent internal consistency in the sample. This suggests that the scale is highly homogeneous.

Additionally, the main domains of the PedsQLTM were evaluated using percentile-transformed scores, categorized into three levels low, moderate and high. These categories were defined by specific intervals: (0.00–33.33), (33.34–66.66) and (66.67–100), respectively. Overall, the domains of the PedsQLTM were evaluated based on these categories. According to the study results, a moderate to low evaluation accounted for the study’s parent-reported QoL and an overall evaluation scored a moderate to low rating. Response rates of parents for the subscale were lowest at pain and hurt (25.67±25.79) and the highest at daily activities (57.05±35.21).
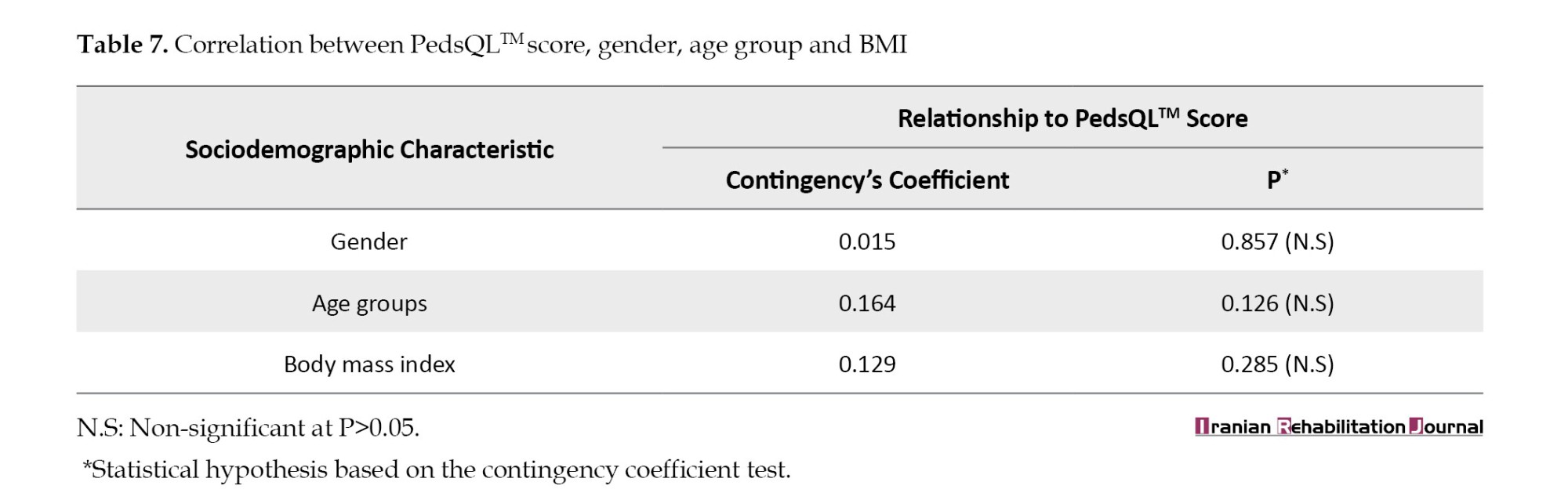
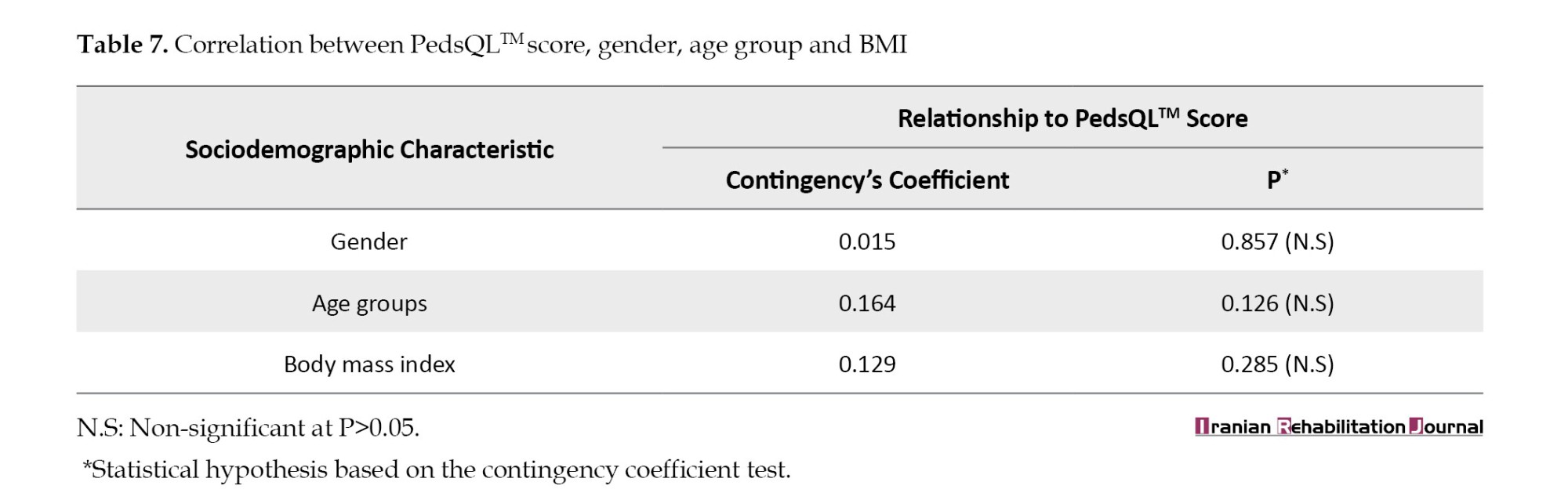
As shown in Table 7, which illustrates contingency coefficients with a testing hypothesis, we attempted to determine the relationship between the overall evaluations of the PedsQLTM score based on the lower and upper cutoff points of the percentile grand mean of parented-reported data and some sociodemographic characteristics (gender, age group and BMI). The findings revealed no significant correlations between the PedsQLTM score and these characteristics.
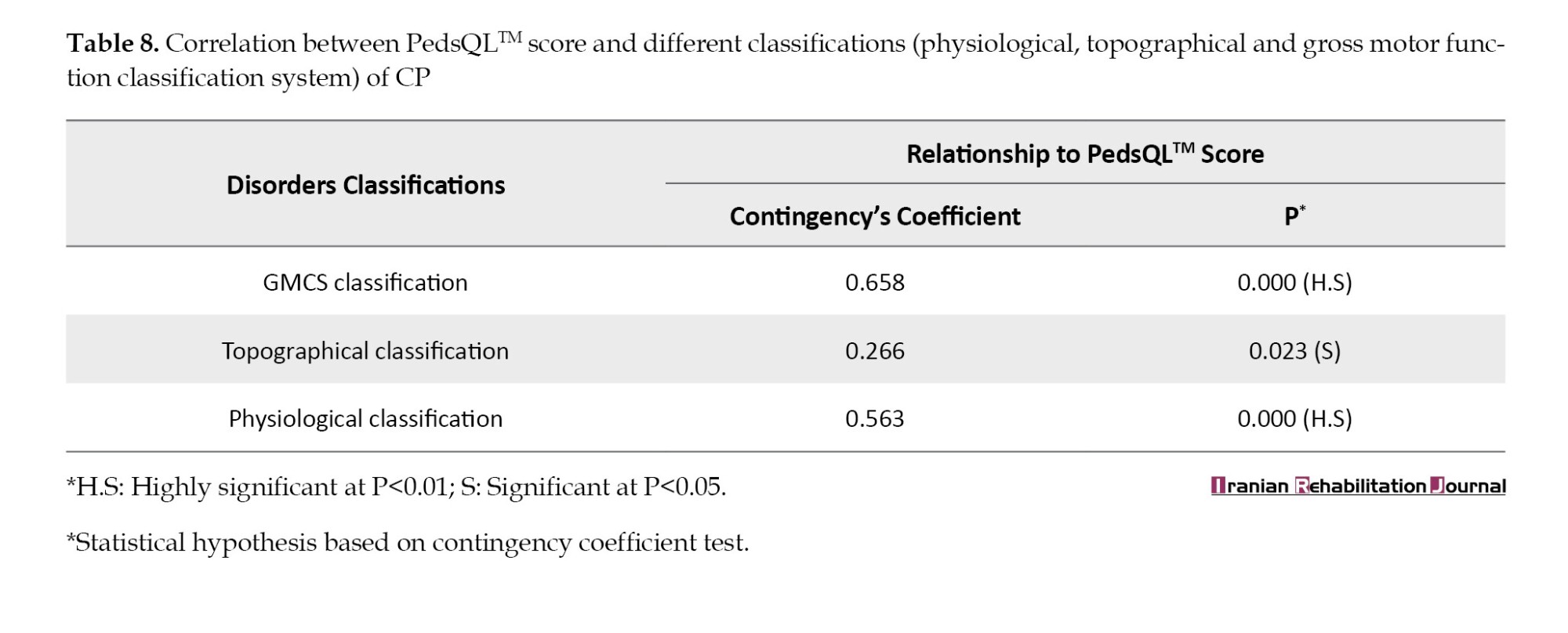
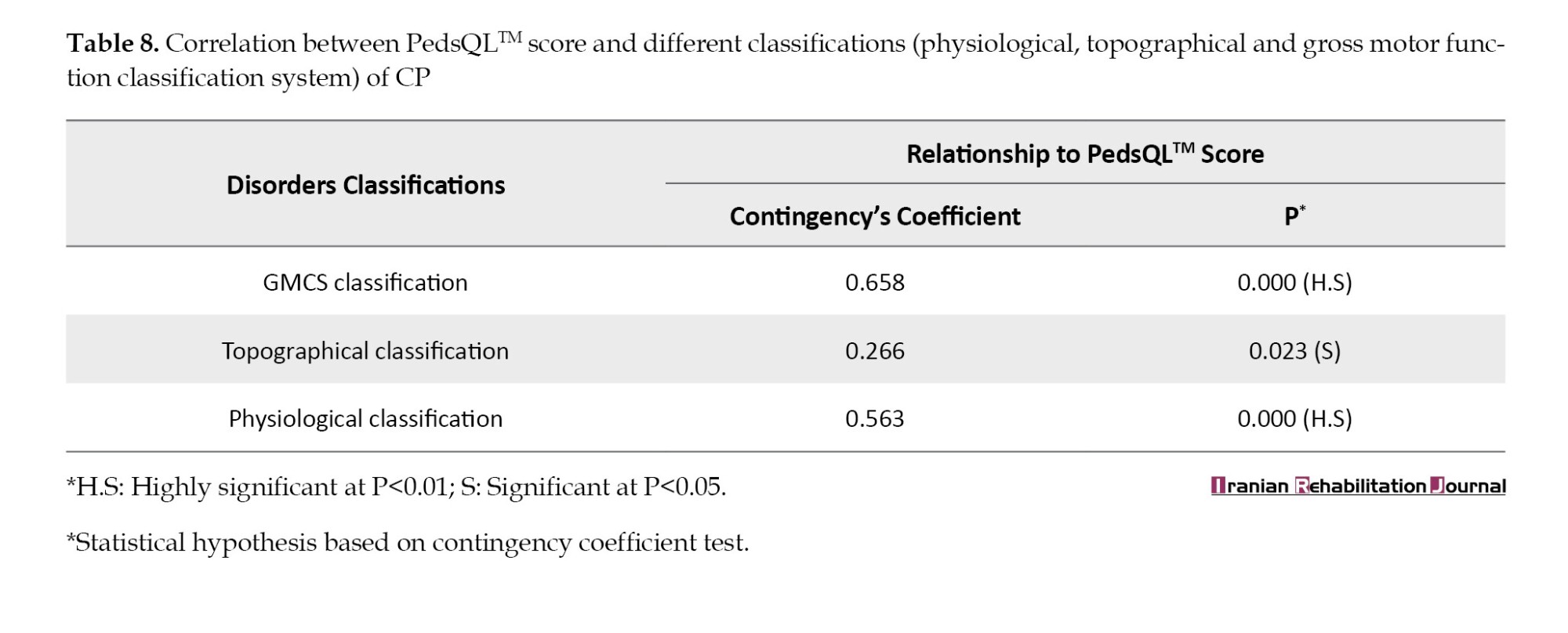
According to the data in Table 8, there is a highly significant correlation between the different classifications of CP (GMCS, topographical, physiological) and the overall PedsQLTM parent-reported QoL with a P<0.000.
Discussion
In most CP research, muscle strength, postural control, range of motion and motor impairments are studied. Only recently has the QoL evaluation become a significant evaluation area for early treatment. Research on the subject is in full swing in foreign countries, but there needs to be more local data available on the subject. Individualized care and support are essential for CP children’s QoL. Mobility, spasticity and fine motor skill issues may greatly impact everyday living. The health-related QoL of children with CP has been the subject of investigation in several research [8-11], while the reported QoL [12-14] has been evaluated in a few studies. All levels of severity have been included in the subjective categories for a sample of children with CP.
Discussion of sociodemographic characteristics of mothers
Current research shows that more than 88.6% of mothers got married before the age of 35 years old, and the Mean±SD were 27.1±6.1 years. The finding matches that of Ali et al. (2022), which indicated that 94.3% of mothers got married before the age of 35 years [15]. No prior research demonstrated that the mother’s age at marriage affects CP risk because numerous other variables influence it. Bleeding during pregnancy, maternal health, and taking medication were identified as risk factors for CP in prenatal. The results obtained from this study showed that (73.8%) did not suffer from bleeding during pregnancy, 68.5% were healthy and did not complain of any diseases and 75.8% did not take medication while pregnant. This research indicated that most mothers of children with CP were healthy, agreeing with Khaleel et al. (2022), who reported that 81.6% had no vaginal hemorrhage during pregnancy, 69.7% were disease-free, and 60.5% did not use medication [16].
Several studies have shed light on the association between cesarean section and CP [17]. Our study revealed that cesarean section was delivered in 62.4% of CP patients. The mother’s history was the only source of information. The reasons for the emergency cesarean section were not explained, nor whether the fetus was in prenatal distress before delivery. Most of these children (92.6%) were born in the hospital, and these findings appear to be consistent with other research that has found that hospitals are the place of birth of most CP children in those studies [16, 18].
Sociodemographic features of children
The majority of youngsters participating in this research, accounting for 55.7%, were male. Similar findings have been found in other studies, showing that CP is more likely to develop in males than in females [12-14], and at preschool age 51.1% with a mean age of 5.7±0.8 years [13]. According to physiological and topographical classification, the commonly observed type of CP children was spastic 81.2% and quadriplegic 47.7%. Several researchers showed that spastic types represented 70% to 80% [12, 13, 19]. The physical abilities of CP children were stratified based on the GMFCS and there were no significant differences among subgroups of children. When a child was found with CP, it was common for the mother or main caretaker to feel more upset as the situation worsened. According to this cross-sectional survey, levels III, IV, and V were assigned to about 59.7% of the youngsters. This finding differed less from Kelvin Yang’s sample [20], which discovered that more than half of the research participants were categorized as levels (IV and V) 59.8%. More than two-thirds of CP children in this research were hospitalized and had kernicterus and hypoxic encephalopathy. All these important risk variables predict impairment and neurodevelopmental delay.
Understanding the symptoms, diagnostic procedures, treatment approaches, and expected outcomes can help parents or caregivers cope and improve. The risk of malnutrition is high for patients with CP [21]. BMI is a simple clinical tool for assessing the patients’ nutritional status [22]. The development of the CP, cognitive, and motor function is delayed in people with significant malnutrition [23]. Our investigation observed that individuals diagnosed with CP had a notably reduced BMI (61.7%), which aligns with the findings reported by Feeley et al. [23].
CP patients’ QoL
The complicated societal issue of CP has repercussions not just for society and for individual families. CP patients’ QoL must be assessed to determine how the illness and treatment affect them. It is regarded as one of the most essential results of treatment and rehabilitation. Neurodevelopmental diseases, such as CP benefit from health-related QoL studies and therapies. Individual physical, mental and social well-being is a health-related QoL [24]. Parents assessed pediatric QoL as low or impaired, with variability across domains, according to our research. Those children’s physical health, emotional perception, social communication, and educational function are all affected. In the current study and comparison with other domains, daily activities had the highest mean value based on the Mean±SD of 57.05±35.21. Research shows that CP youngsters who exercise regularly have a better physical QoL [25]. Children with CP have physical restrictions in mobility and balance, which lowers their QoL. Anxiety and stress have big effects on everyday life. In 2016, a study by Findlay et al. found that pain and getting older were bad for the health-related QoL [26]. Previous research has shown that children diagnosed with CP have significantly worse health-related QoL when they are afflicted by pain, in comparison to their counterparts who do not experience pain that is free of charge [27]. In the world of grief and suffering, there was no zero value, thus there was still hope for answering questions. This research also investigated weariness.
The study found a negative correlation between tiredness severity and physical exercise [28]. However, the causal association between physical exercise and weariness is unclear. It remains uncertain if engaging in physical activity avoids fatigue or whether weariness hinders individuals from participating in physical activity. In adolescents or adults with bilateral CP, the QoL decreases when fatigue increases [29]. Moderate to low were also observed in Mean±SD values in eating activities (34.43±40.39) and the speech and communication domain (30.75±39.26). Several studies using the PedsQLTM 3.0 module for evaluating the quality of life for CP found that children and young adults showed decreased performance levels in daily activities, mobility, balance, speech, and eating [30, 31]. This study investigated the association between several sociodemographic factors, such as gender, age group, and BMI and the overall reported QoL among parents. At a P≤0.05, this study found no statistically significant differences between QoL and these attributes.
Similarly, Mohammed et al. concluded that there is no significant influence of gender on QoL [32]. In addition, Surender et al. (2016) demonstrated a lack of statistically meaningful association between gender/age and QoL [33]. This study contradicts Şimşek et al. (2014), who reported that lower BMI affects health-related QoL for CP children [34]. According to Table 8, there is a correlation between PedsQLTM and the levels of GMFCS, as well as the topographical and physiological classifications. Statistically significant differences were found at P≤0.05. This research confirmed the results of Surender et al. (2016) [33] and Mohammed et al. (2016) [32] that GMFCS severity lowers QoL. In contrast, quadriplegic children exhibited a considerably worse health-related QoL than diplegic and hemiplegic children [35].
Conclusion
This research evaluated the QoL among children diagnosed with CP in Baghdad City, Iraq, marking the first effort of its kind, as far as our current understanding allows us to ascertain. The primary objective of the present research was to assess the health-related QoL of parents of children. Additionally, the study sought to investigate the possible influence of sociodemographic variables, such as gender, age, and BMI, as well as identify any potential factors that might have a detrimental effect on health-related QoL. Children aged 5–7 with CP have low health-related QoL. Linking GMFCS severity, physiological and topographical categorization and health-related QoL. GMFCS is a valid measure of health and QoL. No evidence links age, sex or BMI to life quality. Physical treatment may promote self-esteem, daily living participation, and social engagement in CP patients.
Study limitations
The information about the QoL reported by parents of children diagnosed with CP is often on par with the information supplied by the children themselves. Nevertheless, there are distinctions. Due to their intellectual disabilities and communication difficulties, we could not obtain the children’s reports. The school activities domain was excluded from the questionnaire results since more than half of the participants were of preschool age (5 years), and most children of other ages (6,7 years) were not enrolled in school. Parents’ higher stress levels may affect children’s QoL determination.
Ethical Considerations
Compliance with ethical guidelines
According to letter 81471 from the Baghdad Al-Rusafa Health Directorate, the Research and Development Committee authorized this study on July 6, 2022. A verbal agreement was directly gained from the mothers of the study’s participant children.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors have contributed equally to the implementation of this study.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors sincerely thank all medical staff at the Medical Rehabilitation and Rheumatology Center (MRRC) for their assistance and support.
References
Cerebral palsy (CP) is caused by non-progressive abnormalities in the growing brain of a fetus or child, resulting in movement and posture problems and activity limitations. In addition to motor impairments, CP patients often have sensory, cognitive, communicative, perceptual, and behavioral problems [1]. CP, one of the most common motor disabilities in childhood, is more common in boys than girls due to biological factors, such as a more vulnerable cerebral structure, hormone protective factors, and genetic polymorphism [2], with an estimated average of approximately 3.6 cases per 1000 individuals [3]. CP is a social problem facing society in general and the family in particular and is associated with a variety of social challenges for families and the community. The family may experience more stress because of the children’s need for personal care as well as medical support and protection. CP children have a reduced quality of life (QoL) due to mobility issues and lesser participation in recreational and social activities [4]. World Health Organization (WHO) refers to QoL as a person’s sense of self in light of their culture, value system, goals, expectations, and worries [5]. The perspectives of patients about health-related QoL have considerable importance. QoL evaluations are often used by professionals in the fields of physiotherapy, psychology and social work. The pediatric QoL inventory (PedsQLTM) is one method used tools to assess this aspect of health in young people, whether they are experiencing acute or chronic illness. The WHO suggests measuring a child’s physical, mental, social, and educational involvement using the PedsQLTM 3.0 generic core scales. The QoL of youngsters (aged 5-7 years) was assessed in this study. Recent attention has focused on CP children’s health and QoL. This research used health-related QoL and functional movements to predict social and emotional coping behaviors and the link between QoL and age, gender, and body mass index (BMI). The researchers also want to learn more about the links between the different types of CP categories and patients’ QoL.
Providing well-coordinated and high-quality services focused on their needs encourages social inclusion. It allows them and their families to continue living an everyday life in the community. As the incidence of CP among Iraqi children continues to rise, this study is the first to examine their QoL in Baghdad City, Iraq.
Materials and Methods
This cross-sectional research included CP youngsters and their parents. A pediatric neurologist identified 149 children with CP. They were selected using a nonprobability purposive sampling method from the patients attending the Medical Rehabilitation and Rheumatology Centre. The data were collected from August 2022 to February 2023. This research utilized the Arabic translation of the PedsQLTM 3.0 CP module [6]. Parental reporting for young children (ages 5-7 years) was used instead of a self-completion questionnaire due to intellectual disabilities and communication difficulties in these children [7]. In all patients, mothers completed questionnaires through direct interviews. We obtained a verbal agreement from all the participants. During this study, mothers completed a 35-item (7 domains) questionnaire on the PedsQLTM 3.0 CP module for each child, as well as providing some sociodemographic information about the mother and her health, diseases, or illnesses associated with pregnancy. Additionally, some information about the age, sex, weight, height, mood of delivery, and place of birth was gathered. The gross motor function classification system (GMFCS) for CP was used to categorize functional status according to motor activity. CP children were classified according to physiological and topographic characteristics.
The Arabic iteration of the PedsQLTM 3.0 CP module comprises 35 items further categorized into 7 distinct domains. The framework encompasses several categories, including daily activities, school-related activities, mobility and balance, pain and injury management, weariness, eating activities and speech and communication skills. The scoring system ranges from 0 (indicating the absence of a problem) to 4 (indicating a high frequency of occurrence) as determined by the format, instructions, and the Likert answer scale. The 0-4 scale components are translated to 0-100 for better understanding. If over 50% of the items within the scale are absent, it is not advisable to calculate the scale scores. Meanwhile, higher scores on the scale indicate a greater QoL characterized by a reduced presence of symptoms or challenges. In this given numerical sequence, the values assigned to the numbers 0, 1, 2, 3 and 4 are 100, 75, 50, 25, and 0, respectively. A pilot study was conducted to verify the questionnaire’s reliability, and the final questionnaire was tested on 10 women, yielding the result=0.98, as shown in Table 1. A panel of 10 experts from diverse fields assessed the questionnaire’s validity.
As researchers, we excluded the school activities domain from questionnaire responses since most children involved in the study were not enrolled in schools due to a lack of awareness among parents of the possibility of educating their children, whether in a mainstream or a private school, for children with special needs. The data analyses were performed via the SPSS software, version 26. For categorical variables, descriptive statistics were provided as frequencies and percentages, while for continuous variables, the Mean±SD were determined. Furthermore, substantial comparisons were made to test the reliability of the random distribution hypothesis. The scores were computed based on the PedsQLTM manual. The Cronbach α coefficient was used to conduct reliability analyses based on the average correlation between items, and an interference analysis (contingency coefficient and chi-square) was also conducted to analyze data. The P≤0.05.
Results
Data characteristics of mothers of children
The characteristics of mothers and birth conditions related to CP in children are summarized in Table 2. More than a third, 51(34.3%), of the mothers married at the age between 21-25 years with a mean age of 27.1 years. In addition, over two-thirds, 110(73.8%) of those surveyed reported a normal pregnancy without bleeding. Maternal healthcare during pregnancy showed that more than two-thirds, 102(68.5%), of mothers are healthy, while a minority suffer from hypertension, anemia, asthma, and diabetes mellitus, respectively. While pregnant, the majority of mothers, 113(75.8%), did not take medication during pregnancy. In this study, 93 children (62.4%) were delivered via vaginal delivery and 56(37.6%) were delivered via cesarean section. Almost all the children, 138(92.6%) born in a hospital, and the minority of them, 13(8.7%), have been exposed to trauma at birth or throughout their first year of life.
Sociodemographic characteristics of CP children
According to Table 3, This research included 149 CP patients, with an average age of 5.7±0.8 years, and 83(55.7%) of them were male. Most kids in the oldest age group of 5 years old were not in regular or special education programs, even though just over half of them (51.1%) were old enough to go to school. Nearly 48% of youngsters had quadriplegia and 81.2% of them had spastic CP. The GMFCS classified 38(25.5%) children as level I, followed by 34(22.8%) children as level IV. More than two-thirds of the study cohort (71.80%) had to be admitted to neonatal care facilities, according to our findings. Neonatal jaundice is a known risk factor for CP, and 113 patients (74.8%) in this research exhibited this symptom. Additionally, 101 patients (67.8%) reported experiencing birth asphyxia.
The data reported in Table 4 showed that about two-thirds of the studied sample were underweight (n=92, 61.7%), while 53 cases (36.6%) were registered as normal weight, and only 4(2.7%) were overweight. Among various BMI groups, there were highly significant variations (P=0.01). The preponderance of children with CP who were assessed are underweight, as supported by the results.

As with the parents of children with CP, QoL was assessed in six different areas. The evaluation did not include academic assignments but rather encompassed different aspects, such as everyday activities, physical coordination and stability, discomfort and discomfort, exhaustion, dietary habits, and verbal expression and communication. On a four-category scale with scores of (0, 1, 2, 3 and 4), “never,” “always,” “never,” “sometimes,” “often” and “almost always” were assigned to each area. Table 5 summarizes the initial assessment statistics, including Mean±SD score, and relative adequacy. Scores are categorized into three levels low, medium, and high, depending on their transferred scores and their relative adequacy intervals ([0.00-33.33], [33.34-66.66], [66.67-100]).

Based on the results of Table 5, seven items within the domain of daily activities are evaluated at a moderate level (77.78%) and 2 items at a high level (22.22%). In the movement and balance domain, 3(60.0%) items are evaluated at a moderate level and 1(20.0) item is evaluated at a high and low level. In the response to the pain and aches domain, 3(60.0%) items are rated moderately, 1(20.0) item is rated high, and 1(20.0) item is rated low. In the fatigue domain, all items are rated low. Meanwhile, in the eating activities domain, 3(60%) items rated moderate level and 2(40%) items at a low level. Lastly, in the speech and communicate domain, 2(50%) items were rated low, and 2(50%) items were rated moderate. According to the findings of prior research, the QoL of the parents was shown to have a negative correlation with the health-related QoL of their CP children. This association was mostly the result of the research having a mediocre to bad evaluation of the majority of the items.
The PedsQLTM 3.0 CP module’s first findings were obtained through parents’ reports. These findings are provided in Table 6, which includes the percentile grand mean score, pooled standard deviation and reliability for each subscale. The consistency of the results across all of the subscales was used to evaluate the dependability of the measurements. The Cronbach α coefficient of 0.905 indicates that the PedsQLTM scale exhibited excellent internal consistency in the sample. This suggests that the scale is highly homogeneous.

Additionally, the main domains of the PedsQLTM were evaluated using percentile-transformed scores, categorized into three levels low, moderate and high. These categories were defined by specific intervals: (0.00–33.33), (33.34–66.66) and (66.67–100), respectively. Overall, the domains of the PedsQLTM were evaluated based on these categories. According to the study results, a moderate to low evaluation accounted for the study’s parent-reported QoL and an overall evaluation scored a moderate to low rating. Response rates of parents for the subscale were lowest at pain and hurt (25.67±25.79) and the highest at daily activities (57.05±35.21).
As shown in Table 7, which illustrates contingency coefficients with a testing hypothesis, we attempted to determine the relationship between the overall evaluations of the PedsQLTM score based on the lower and upper cutoff points of the percentile grand mean of parented-reported data and some sociodemographic characteristics (gender, age group and BMI). The findings revealed no significant correlations between the PedsQLTM score and these characteristics.
According to the data in Table 8, there is a highly significant correlation between the different classifications of CP (GMCS, topographical, physiological) and the overall PedsQLTM parent-reported QoL with a P<0.000.
Discussion
In most CP research, muscle strength, postural control, range of motion and motor impairments are studied. Only recently has the QoL evaluation become a significant evaluation area for early treatment. Research on the subject is in full swing in foreign countries, but there needs to be more local data available on the subject. Individualized care and support are essential for CP children’s QoL. Mobility, spasticity and fine motor skill issues may greatly impact everyday living. The health-related QoL of children with CP has been the subject of investigation in several research [8-11], while the reported QoL [12-14] has been evaluated in a few studies. All levels of severity have been included in the subjective categories for a sample of children with CP.
Discussion of sociodemographic characteristics of mothers
Current research shows that more than 88.6% of mothers got married before the age of 35 years old, and the Mean±SD were 27.1±6.1 years. The finding matches that of Ali et al. (2022), which indicated that 94.3% of mothers got married before the age of 35 years [15]. No prior research demonstrated that the mother’s age at marriage affects CP risk because numerous other variables influence it. Bleeding during pregnancy, maternal health, and taking medication were identified as risk factors for CP in prenatal. The results obtained from this study showed that (73.8%) did not suffer from bleeding during pregnancy, 68.5% were healthy and did not complain of any diseases and 75.8% did not take medication while pregnant. This research indicated that most mothers of children with CP were healthy, agreeing with Khaleel et al. (2022), who reported that 81.6% had no vaginal hemorrhage during pregnancy, 69.7% were disease-free, and 60.5% did not use medication [16].
Several studies have shed light on the association between cesarean section and CP [17]. Our study revealed that cesarean section was delivered in 62.4% of CP patients. The mother’s history was the only source of information. The reasons for the emergency cesarean section were not explained, nor whether the fetus was in prenatal distress before delivery. Most of these children (92.6%) were born in the hospital, and these findings appear to be consistent with other research that has found that hospitals are the place of birth of most CP children in those studies [16, 18].
Sociodemographic features of children
The majority of youngsters participating in this research, accounting for 55.7%, were male. Similar findings have been found in other studies, showing that CP is more likely to develop in males than in females [12-14], and at preschool age 51.1% with a mean age of 5.7±0.8 years [13]. According to physiological and topographical classification, the commonly observed type of CP children was spastic 81.2% and quadriplegic 47.7%. Several researchers showed that spastic types represented 70% to 80% [12, 13, 19]. The physical abilities of CP children were stratified based on the GMFCS and there were no significant differences among subgroups of children. When a child was found with CP, it was common for the mother or main caretaker to feel more upset as the situation worsened. According to this cross-sectional survey, levels III, IV, and V were assigned to about 59.7% of the youngsters. This finding differed less from Kelvin Yang’s sample [20], which discovered that more than half of the research participants were categorized as levels (IV and V) 59.8%. More than two-thirds of CP children in this research were hospitalized and had kernicterus and hypoxic encephalopathy. All these important risk variables predict impairment and neurodevelopmental delay.
Understanding the symptoms, diagnostic procedures, treatment approaches, and expected outcomes can help parents or caregivers cope and improve. The risk of malnutrition is high for patients with CP [21]. BMI is a simple clinical tool for assessing the patients’ nutritional status [22]. The development of the CP, cognitive, and motor function is delayed in people with significant malnutrition [23]. Our investigation observed that individuals diagnosed with CP had a notably reduced BMI (61.7%), which aligns with the findings reported by Feeley et al. [23].
CP patients’ QoL
The complicated societal issue of CP has repercussions not just for society and for individual families. CP patients’ QoL must be assessed to determine how the illness and treatment affect them. It is regarded as one of the most essential results of treatment and rehabilitation. Neurodevelopmental diseases, such as CP benefit from health-related QoL studies and therapies. Individual physical, mental and social well-being is a health-related QoL [24]. Parents assessed pediatric QoL as low or impaired, with variability across domains, according to our research. Those children’s physical health, emotional perception, social communication, and educational function are all affected. In the current study and comparison with other domains, daily activities had the highest mean value based on the Mean±SD of 57.05±35.21. Research shows that CP youngsters who exercise regularly have a better physical QoL [25]. Children with CP have physical restrictions in mobility and balance, which lowers their QoL. Anxiety and stress have big effects on everyday life. In 2016, a study by Findlay et al. found that pain and getting older were bad for the health-related QoL [26]. Previous research has shown that children diagnosed with CP have significantly worse health-related QoL when they are afflicted by pain, in comparison to their counterparts who do not experience pain that is free of charge [27]. In the world of grief and suffering, there was no zero value, thus there was still hope for answering questions. This research also investigated weariness.
The study found a negative correlation between tiredness severity and physical exercise [28]. However, the causal association between physical exercise and weariness is unclear. It remains uncertain if engaging in physical activity avoids fatigue or whether weariness hinders individuals from participating in physical activity. In adolescents or adults with bilateral CP, the QoL decreases when fatigue increases [29]. Moderate to low were also observed in Mean±SD values in eating activities (34.43±40.39) and the speech and communication domain (30.75±39.26). Several studies using the PedsQLTM 3.0 module for evaluating the quality of life for CP found that children and young adults showed decreased performance levels in daily activities, mobility, balance, speech, and eating [30, 31]. This study investigated the association between several sociodemographic factors, such as gender, age group, and BMI and the overall reported QoL among parents. At a P≤0.05, this study found no statistically significant differences between QoL and these attributes.
Similarly, Mohammed et al. concluded that there is no significant influence of gender on QoL [32]. In addition, Surender et al. (2016) demonstrated a lack of statistically meaningful association between gender/age and QoL [33]. This study contradicts Şimşek et al. (2014), who reported that lower BMI affects health-related QoL for CP children [34]. According to Table 8, there is a correlation between PedsQLTM and the levels of GMFCS, as well as the topographical and physiological classifications. Statistically significant differences were found at P≤0.05. This research confirmed the results of Surender et al. (2016) [33] and Mohammed et al. (2016) [32] that GMFCS severity lowers QoL. In contrast, quadriplegic children exhibited a considerably worse health-related QoL than diplegic and hemiplegic children [35].
Conclusion
This research evaluated the QoL among children diagnosed with CP in Baghdad City, Iraq, marking the first effort of its kind, as far as our current understanding allows us to ascertain. The primary objective of the present research was to assess the health-related QoL of parents of children. Additionally, the study sought to investigate the possible influence of sociodemographic variables, such as gender, age, and BMI, as well as identify any potential factors that might have a detrimental effect on health-related QoL. Children aged 5–7 with CP have low health-related QoL. Linking GMFCS severity, physiological and topographical categorization and health-related QoL. GMFCS is a valid measure of health and QoL. No evidence links age, sex or BMI to life quality. Physical treatment may promote self-esteem, daily living participation, and social engagement in CP patients.
Study limitations
The information about the QoL reported by parents of children diagnosed with CP is often on par with the information supplied by the children themselves. Nevertheless, there are distinctions. Due to their intellectual disabilities and communication difficulties, we could not obtain the children’s reports. The school activities domain was excluded from the questionnaire results since more than half of the participants were of preschool age (5 years), and most children of other ages (6,7 years) were not enrolled in school. Parents’ higher stress levels may affect children’s QoL determination.
Ethical Considerations
Compliance with ethical guidelines
According to letter 81471 from the Baghdad Al-Rusafa Health Directorate, the Research and Development Committee authorized this study on July 6, 2022. A verbal agreement was directly gained from the mothers of the study’s participant children.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors have contributed equally to the implementation of this study.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors sincerely thank all medical staff at the Medical Rehabilitation and Rheumatology Center (MRRC) for their assistance and support.
References
- Rosenbaum, P. A report: The definition and classification of cerebral palsy April 2006. Developmental Medicine & Child Neurology. 2007; 49(suppl 109):8-14. [DOI:10.1111/j.1469-8749.2007.tb12610.x]
- Romeo DM, Sini F, Brogna C, Albamonte E, Ricci D, Mercuri E. Sex differences in cerebral palsy on neuromotor outcome: A critical review. Developmental Medicine & Child Neurology. 2016; 58(8):809-13. [DOI:10.1111/dmcn.13137] [PMID]
- Yeargin-Allsopp M, Van Naarden Braun K, Doernberg NS, Benedict RE, Kirby RS, Durkin MS. Prevalence of cerebral palsy in 8-year-old children in three areas of the United States in 2002: A multisite collaboration. Pediatrics. 2008; 121(3):547-54. [DOI:10.1542/peds.2007-1270] [PMID]
- King G, Tucker MA, Baldwin P, Lowry K, LaPorta J, Martens L. A life needs model of pediatric service delivery: Services to support community participation and quality of life for children and youth with disabilities. Physical & Occupational Therapy in Pediatrics. 2002; 22(2):53-77. [DOI:10.1080/J006v22n02_04]
- No Author. The World Health Organization quality of life assessment (WHOQOL): Position paper from the World Health Organization. 1995; 41(10):1403-9. [DOI:10.1016/0277-9536(95)00112-K] [PMID]
- Almuwais A, Alzahrani N, Almuhalhil M, Adossary S, Alyagoot S, Alqabbani S. Agreement between Saudi children with cerebral palsy and their parents on™ 3.0: A pilot study. Current Pediatric Research. 2021; 25(3): 387-92. [Link]
- Varni JW, Burwinkle TM, Berrin SJ, Sherman SA, Artavia K, Malcarne VL, et al. The PedsQL in pediatric cerebral palsy: Reliability, validity, and sensitivity of the Generic Core Scales and Cerebral Palsy Module. Developmental Medicine and Child Neurology. 2006; 48(6):442-9. [PMID]
- Bjornson KF, McLaughlin JF. The measurement of health-related quality of life (HRQL) in children with cerebral palsy. European Journal of Neurology. 2001; 8(Suppl 5):183-93. [DOI:10.1046/j.1468-1331.2001.00051.x] [PMID]
- Rosenbaum PL, Livingston MH, Palisano RJ, Galuppi BE, Russell DJ. Quality of life and health-related quality of life of adolescents with cerebral palsy. Developmental Medicine and Child Neurology. 2007; 49(7):516-21. [DOI:10.1111/j.1469-8749.2007.00516.x] [PMID]
- Dobhal M, Juneja M, Jain R, Sairam S, Thiagarajan D. Health-related quality of life in children with cerebral palsy and their families. Indian Pediatrics. 2014; 51(5):385-7. [DOI:10.1007/s13312-014-0414-z] [PMID]
- Ko JY, Lee BH, Kim MY. Health-related quality of life in children with severe cerebral palsy. Journal of the Korean Academy of Rehabilitation Medicine. 2009; 33(4):415-22. [Link]
- Arnaud C, White-Koning M, Michelsen SI, Parkes J, Parkinson K, Thyen U, et al. Parent-reported quality of life of children with cerebral palsy in Europe. Pediatrics. 2008; 121(1):54-64. [DOI:10.1542/peds.2007-0854] [PMID]
- Hasan S, Shaker N, Ismail Z. Impact of spastic cerebral palsy upon the quality of life of children under the age of 12 years in Erbil City: Parents’ reports. Iraqi National Journal of Nursing Specialties. 2015; 28(1):8-16. [DOI:10.58897/injns.v28i1.214]
- Vargus-Adams J. Health-related quality of life in childhood cerebral palsy. Archives of Physical Medicine and Rehabilitation. 2005; 86(5):940-5. [DOI:10.1016/j.apmr.2004.10.036] [PMID]
- Ali TA, Ali SB, Ali MA. Assessment of nutritional status for Sudanese children with cerebral Palsy in two rehabilitation centers in Khartoum state, Sudan. Journal of the Saudi Society for Food and Nutrition (JSSFN). 2022; 15(1):87-96. [Link]
- Khaleel RF, Abdul-Aziz RM, Katea SS. A clinicoepidemiological study of cerebral palsy among children attending Medical Rehabilitation and Rheumatology Center. Medical Journal of Babylon. 2022; 19(4):664-70. [DOI: 10.4103/MJBL.MJBL_205_22]
- Jacobsson B, Hagberg G, Hagberg B, Ladfors L, Niklasson A, Hagberg H. Cerebral palsy in preterm infants: A population-based case-control study of antenatal and intrapartal risk factors. Acta Paediatrica. 2002; 91(8):946-51. [DOI:10.1080/080352502760148685] [PMID]
- Keramat KU, Khalily MA, Bhutta AH, Khattak P, Habib A, Bhutta NI. Risk factors evaluation of cerebral palsy in Hazara division Khyber Pakhtunkhwa Pakistan: A cross-sectional survey. The Journal of the Pakistan Medical Association. 2022; 72(7):1315-9. [DOI:10.47391/JPMA.1669] [PMID]
- Mu’ala EA, Rabati AA, Shwani SS. Psychological burden of a child with Cerebral Palsy upon caregivers in Erbil Governorate. Iraqi Postgraduate Medical Journal. 2008; 7(2):129-34. [Link]
- Ying K, Rostenberghe HV, Kuan G, Mohd Yusoff MHA, Ali SH, Yaacob NS. Health-related quality of life and family functioning of primary caregivers of children with cerebral palsy in Malaysia. International Journal of Environmental Research and Public Health. 2021; 18(5):2351. [DOI:10.3390/ijerph18052351] [PMID]
- González L, Nazario CM, González MJ. Nutrition-related problems of pediatric patients with neuromuscular disorders. Puerto Rico Health Sciences Journal. 2000; 19(1):35-8. [PMID]
- Pietrobelli A, Faith MS, Allison DB, Gallagher D, Chiumello G, Heymsfield SB. Body mass index as a measure of adiposity among children and adolescents: A validation study. The Journal of Pediatrics. 1998; 132(2):204-10. [DOI:10.1016/S0022-3476(98)70433-0] [PMID]
- Feeley BT, Gollapudi K, Otsuka NY. Body mass index in ambulatory cerebral palsy patients. Journal of Pediatric Orthopedics. Part B. 2007; 16(3):165-9. [DOI:10.1097/01.bpb.0000236230.44819.95] [PMID]
- Solans M, Pane S, Estrada MD, Serra-Sutton V, Berra S, Herdman M, et al. Health-related quality of life measurement in children and adolescents: A systematic review of generic and disease-specific instruments. Value in health. 2008; 11(4):742-64. [DOI:10.1111/j.1524-4733.2007.00293.x] [PMID]
- Maher CA, Toohey M, Ferguson M. Physical activity predicts quality of life and happiness in children and adolescents with cerebral palsy. Disability and Rehabilitation. 2016; 38(9):865-9. [DOI:10.3109/09638288.2015.1066450] [PMID]
- Findlay B, Switzer L, Narayanan U, Chen S, Fehlings D. Investigating the impact of pain, age, Gross Motor Function Classification System, and sex on health-related quality of life in children with cerebral palsy. Developmental Medicine and Child Neurology. 2016; 58(3):292-7. [DOI:10.1111/dmcn.12936] [PMID]
- Russo RN, Miller MD, Haan E, Cameron ID, Crotty M. Pain characteristics and their association with quality of life and self-concept in children with hemiplegic cerebral palsy identified from a population register. The Clinical Journal of Pain. 2008; 24(4):335-42. [DOI:10.1097/AJP.0b013e318162eae0] [PMID]
- McPhee PG, Brunton LK, Timmons BW, Bentley T, Gorter JW. Fatigue and its relationship with physical activity, age, and body composition in adults with cerebral palsy. Developmental Medicine and Child Neurology. 2017; 59(4):367-73.[DOI:10.1111/dmcn.13306] [PMID]
- Lundh S, Nasic S, Riad J. Fatigue, quality of life and walking ability in adults with cerebral palsy. Gait & Posture. 2018; 61:1-6. [DOI:10.1016/j.gaitpost.2017.12.017] [PMID]
- Lewicka M, Kurylak A. Assessment of quality of life in patients with cerebral palsy. Pediatria Polska-Polish Journal of Paediatrics. 2019; 94(2):119-27. [DOI:10.5114/polp.2019.85041]
- Yang X, Xiao N, Yan J. The PedsQL in pediatric cerebral palsy: Reliability and validity of the Chinese version pediatric quality of life inventory 4.0 generic core scales and 3.0 cerebral palsy module. Quality of Life Research. 2011; 20(2):243-52. [DOI: 10.1007/s11136-010-9751-0] [PMID]
- Mohammed FM, Ali SM, Mustafa MA. Quality of life of cerebral palsy patients and their caregivers: A cross sectional study in a rehabilitation center Khartoum-Sudan (2014 - 2015). Journal of Neurosciences in Rural Practice. 2016; 7(3):355-61. [DOI: 10.4103/0976-3147.182778] [PMID]
- Surender S, Gowda VK, Sanjay KS, Basavaraja GV, Benakappa N, Benakappa A. Caregiver-reported health-related quality of life of children with cerebral palsy and their families and its association with gross motor function: A South Indian study. Journal of Neurosciences in Rural Practice. 2016; 7(02):223-7. [DOI:10.4103/0976-3147.178657] [PMID]
- Şimşek TT, Tuç G. Examination of the relation between body mass index, functional level and health-related quality of life in children with cerebral palsy. Turk Pediatri Arsivi. 2014; 49(2):130-7. [DOI:10.5152/tpa.2014.1238] [PMID]
- Varni JW, Burwinkle TM, Sherman SA, Hanna K, Berrin SJ, Malcarne VL, et al. Health-related quality of life of children and adolescents with cerebral palsy: Hearing the voices of the children. Developmental Medicine and Child Neurology. 2005; 47(9):592-7. [DOI:10.1111/j.1469-8749.2005.tb01209.x]
Article type: Original Research Articles |
Subject:
Social Welfare
Received: 2023/06/15 | Accepted: 2023/09/12 | Published: 2024/06/1
Received: 2023/06/15 | Accepted: 2023/09/12 | Published: 2024/06/1
Send email to the article author